Menopause is a natural stage in a woman's life, yet it can often feel overwhelming due to the multitude of changes occurring within the body. This guide aims to provide an in-depth understanding of menopause, its stages, symptoms, and the various treatment options available. Drawing insights from respected experts in functional medicine, Dr. Lara Briden and Dr. Jolene Brighten, we will explore both conventional and natural approaches to managing menopause.
What is Menopause and When Does it Typically Occur?
Menopause marks the end of a woman's reproductive years, characterised by the cessation of menstruation. It typically occurs between the ages of 45 and 55, with the average age being around 51 in the UK (1). However, some women may experience menopause earlier due to genetic factors, medical conditions, or surgical procedures (e.g., hysterectomy).
Testing for Perimenopause, and Menopause
Determining if someone has entered perimenopause is complex, as there is no single test for it. The transition to menopause is gradual and hormone levels can vary unpredictably. Therefore, doctors consider a range of factors such as age, menstrual history, and symptoms to diagnose perimenopause. Common symptoms include irregular periods, hot flashes, and sleep disturbances.
A healthcare professional can determine if a woman is experiencing menopause by conducting blood or urine tests to measure hormone levels. These tests can assess the levels of:
Estradiol
This hormone's levels decline around the time of menopause and become undetectable after menopause.
Follicle-stimulating hormone (FSH)
FSH levels rise as menopause approaches. The brain produces FSH to prompt the ovaries to produce estrogen. However, FSH levels can vary throughout the menstrual cycle.
Stages of Menopause
Menopause is not a singular event but a series of stages that can span several years:
1. Perimenopause
This transitional phase can begin as early as the mid-30s, lasting until menopause occurs. During perimenopause, hormone levels fluctuate significantly, leading to irregular menstrual cycles and various symptoms (2).
2. Menopause
Menopause is officially diagnosed when a woman has not had a menstrual period for 12 consecutive months. This stage signifies a significant decrease in oestrogen production (3).
3. Postmenopause
This stage begins after menopause and lasts for the rest of a woman's life. Symptoms may ease for some, while others may continue to experience menopausal symptoms related to lower hormone levels (4).
Common Symptoms and How to Manage Them
Women may experience a variety of symptoms during menopause, including (5):
- Hot flashes
- Night sweats
- Mood swings
- Vaginal dryness
- Sleep disturbances
- Weight gain
- Changes in libido
Conventional HRT vs. Bioidentical HRT
Hormone Replacement Therapy (HRT) is commonly prescribed to manage menopausal symptoms, but it’s essential to differentiate between conventional HRT and bioidentical HRT (BHRT).
Conventional HRT
This approach typically uses synthetic hormones derived from pregnant mares' urine or manufactured in laboratories. While it can be effective for some, many women experience side effects, including bloating, headaches, unexpected vaginal bleeding, mood changes including low mood and depression, diarrhoea, hair loss, and an increased risk of certain health conditions (6).
Bioidentical HRT
In contrast, BHRT utilises hormones that are chemically identical to those produced by the human body, making them more compatible and often better tolerated. Dr. Jolene Brighten advocates for the use of BHRT, citing its safety and efficacy in managing menopausal symptoms with fewer side effects (7).
Further Natural Remedies and Lifestyle Changes
In addition to BHRT options, many women seek natural remedies to alleviate menopausal symptoms. Consider implementing the following:
- Herbal Supplements: Herbs such as black cohosh and red clover have been traditionally used for their potential to alleviate hot flashes and other menopause-related symptoms. Black cohosh, in particular, may help regulate hormonal fluctuations (8), while red clover is rich in phytoestrogens that can mimic estrogen in the body (9), providing relief for many women experiencing these changes.
- Acupuncture: This ancient practice of traditional Chinese medicine involves the insertion of fine needles into specific points on the body. It has shown promising results in reducing the frequency and intensity of hot flashes, as well as improving overall mood and well-being (10). Many women report a greater sense of balance and calm after undergoing acupuncture treatments, making it a valuable option for managing menopausal symptoms.
- Mind-Body Practices: Techniques such as yoga and meditation focus on the connection between the mind and body, promoting relaxation and stress reduction. Regular practice of yoga can enhance flexibility and strength (11), while also fostering mindfulness, which has been linked to improved hormonal balance. Meditation, on the other hand, helps to quiet the mind, reduce anxiety (12), and cultivate a sense of inner peace, all of which can be beneficial during the transition of menopause.
Functional Medicine Approach to Menopause
Functional medicine takes a holistic view of health, focusing on identifying and addressing the root causes of symptoms rather than merely treating them. Both Dr. Briden and Dr. Brighten advocate for this approach:
- Individualised Treatment Plans: Each woman’s experience with menopause is unique, with diverse symptoms and challenges that can vary widely from one individual to another. Functional medicine practitioners take a comprehensive approach by thoroughly assessing each woman's health history, lifestyle choices, and environmental factors. This in-depth evaluation enables them to create highly tailored treatment plans that address specific needs and promote overall well-being during this transitional phase of life.
- Gut Health: Dr. Brighten emphasizes the crucial connection between gut health and hormonal balance, highlighting that a well-functioning digestive system plays a significant role in the body’s hormonal regulation (13). She suggests that maintaining a healthy gut, through a balanced diet rich in probiotics and fiber, can lead to improvements in menopausal symptoms. By supporting gut health, women may experience reduced hormonal fluctuations, enhanced mood stability, and overall better management of menopausal challenges.
Expert Insights on Managing Menopause Symptoms Naturally

Both Dr. Briden and Dr. Brighten have shared valuable insights regarding effective natural management of menopausal symptoms.
- Nutrition: Dr. Briden emphasizes the crucial role of nutrition in achieving hormone balance during menopause. Incorporating a variety of foods rich in healthy fats, fiber, and antioxidants not only supports overall health but also alleviates some menopausal symptoms. Foods like avocados, nuts, seeds, and leafy greens can be particularly beneficial, helping to stabilize energy levels and improve mood (14).
- Gut Health: According to Dr. Brighton, maintaining gut health and addressing inflammation is vital for effectively managing menopause symptoms. Probiotics and prebiotics can play a significant role in sustaining a healthy gut flora, which is essential for hormone regulation and overall well-being (15). Foods such as yogurt, fermented vegetables, and whole grains can help nourish beneficial gut bacteria, leading to improved digestion and reduced inflammation (16).
- Physical Activity and Sleep: Both experts highlight the importance of engaging in regular physical activity and prioritizing quality sleep to enhance overall quality of life during menopause. Exercise can help reduce stress, improve mood, and maintain a healthy weight (17), while adequate sleep is necessary for hormone regulation and recovery (18). Incorporating activities like walking, yoga, or strength training, along with establishing a calming bedtime routine, can significantly contribute to better health during this transition.
Nutritional Needs During Perimenopause and Menopause
Navigating the stages of perimenopause and menopause can be a challenging experience. These life transitions bring about significant hormonal changes that can impact your overall health and well-being. One area that often requires attention is nutrition. Understanding common nutrient deficiencies and extra nutritional needs during these phases can help you maintain optimal health and manage symptoms more effectively.
Common Nutrient Deficiencies During Perimenopause and Menopause
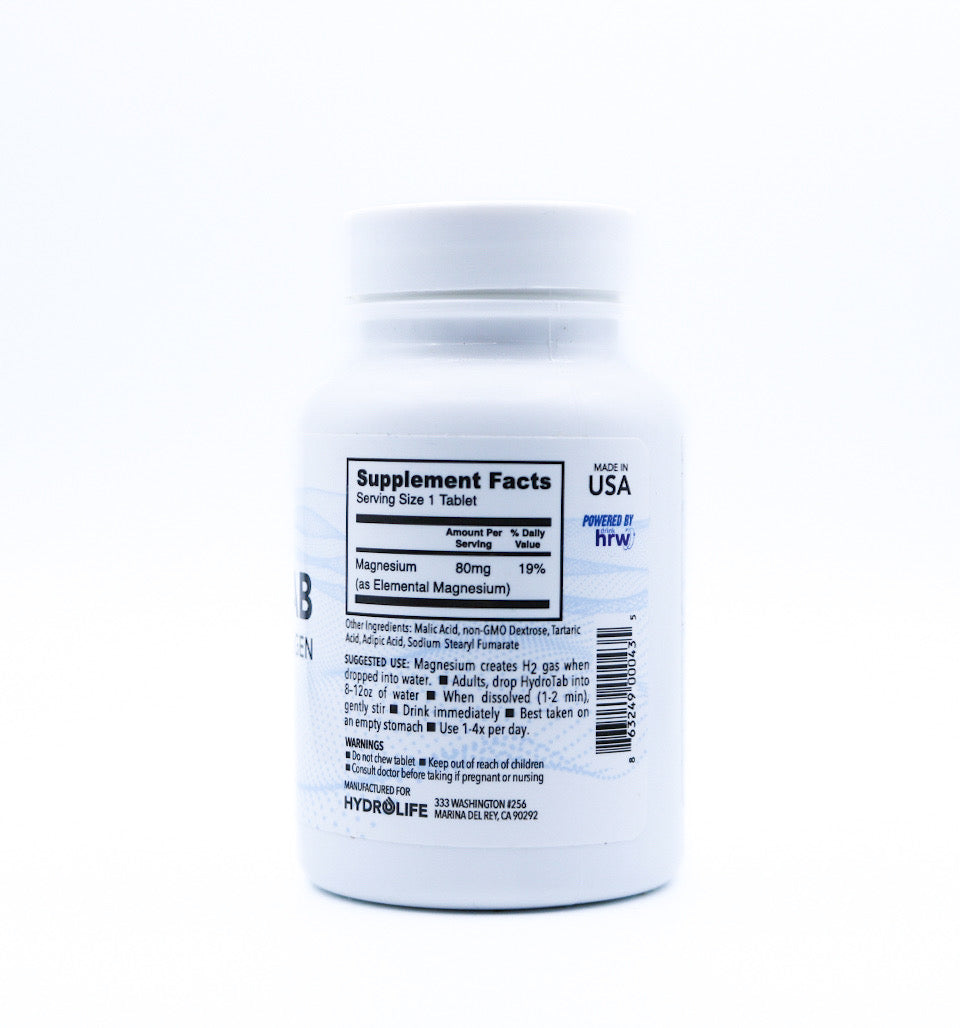
1. Calcium & Magnesium
Hormonal changes during menopause can lead to a decrease in bone density, increasing the risk of osteoporosis. This is mostly due to the lowered levels of oestrogen (19). Calcium and magnesium are both crucial for maintaining strong bones (20). Women in perimenopause and menopause should aim to get enough calcium and magnesium through their diet and supplements if necessary. Magnesium also aids in sleep, and helps regulate muscle and nerve function (21). A deficiency can exacerbate symptoms like cramps, insomnia, and mood swings.
Sources of Calcium (22):
- Dairy products like milk, cheese, and yoghurt
- Leafy green vegetables such as kale and spinach
- Fortified foods like orange juice and cereals
Sources of Magnesium (23):

- Plant foods: Legumes, dark green leafy vegetables, nuts, seeds, whole grains, and fortified cereals. Some specific examples include:
- Leafy greens: Spinach and kale
- Nuts and seeds: Almonds, cashews, and pumpkin seeds
- Whole grains: Quinoa and brown rice
- Fruits: Avocados, bananas, apples, and papayas
2. Vitamin D
Vitamin D enhances calcium absorption and plays a critical role in bone health (24). Due to reduced sun exposure and aging, many women may experience a deficiency in vitamin D during menopause.
Sources of Vitamin D (25):
- Sunlight exposure
- Fatty fish like salmon and mackerel
- Fortified foods and supplements
4. Vitamin B12
Vitamin B12 is essential for energy production and cognitive function (26). Absorption of B12 can decrease with age, making it important to monitor intake during menopause.
Sources of Vitamin B12 (26):
- Meat, fish, and poultry
- Eggs and dairy products
- Fortified cereals
5. Iron
While the risk of iron deficiency decreases post-menopause due to the cessation of menstruation, some women still struggle with low iron levels. Iron is vital for oxygen transport in the blood and energy levels.
Sources of Iron (27):
- Red meat and poultry
- Beans and lentils
- Spinach and fortified cereals
Extra Nutritional Needs During Perimenopause and Menopause
1. Phytoestrogens
Phytoestrogens are plant-based compounds that can mimic the effects of estrogen in the body. They may help alleviate some menopausal symptoms such as hot flashes and night sweats (28).
Sources of Phytoestrogens (29):
- Soy products like tofu and tempeh
- Flaxseeds
- Legumes
2. Healthy Fats
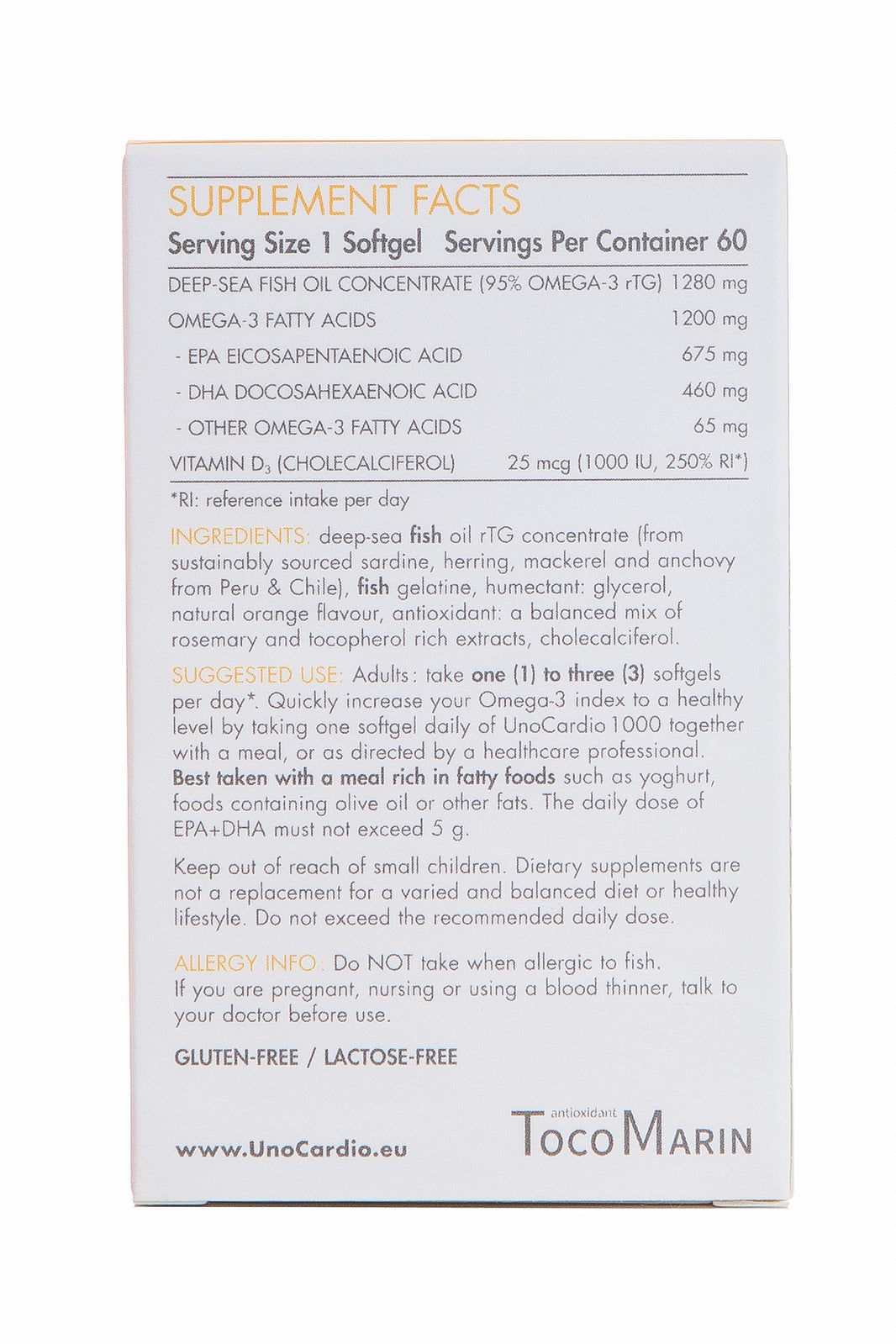
Omega-3 fatty acids have anti-inflammatory properties and support heart health, which is crucial as the risk of cardiovascular diseases increases post-menopause (30).
Sources of Healthy Fats (31):
- Fatty fish such as salmon, mackerel, and sardines
- Chia seeds and flaxseeds
- Walnuts
3. Fibre
Fibre is important for digestive health and can help manage weight by promoting a feeling of fullness. It can also aid in controlling blood sugar levels and lowering cholesterol (32).
Sources of Fibre (33):
- Whole grains like oats, barley, and quinoa
- Fruits like apples, berries, and pears
- Vegetables such as broccoli and carrots
4. Protein
Adequate protein intake is essential for maintaining muscle mass, which can diminish with age. It also supports overall metabolic health (34).
Sources of Protein (35):
- Lean meats like chicken and turkey
- Fish and seafood
- Plant-based proteins like beans, lentils, and chickpeas
Perimenopause and menopause are periods of significant change, but with the right nutritional support, you can manage symptoms and maintain your health. Paying attention to common nutrient deficiencies and incorporating foods rich in essential vitamins and minerals can make a substantial difference in your well-being.
Health Advice for a Smoother Menopausal Transition
Navigating menopause can be challenging, but with the right support and knowledge, it can be a smoother transition. Here are some actionable tips:
- Stay Informed: Educate yourself about menopause through reputable resources, forums, and workshops.
- Connect with Others: Join support groups or online communities where you can share experiences and advice with other women going through similar changes.
- Consult Healthcare Professionals: Work with healthcare providers who understand menopause and can guide you through treatment options.
UK Support Networks and Resources
Women in the UK have access to various resources and support networks:
- Menopause Matters - A dedicated website offering information, forums, and support for women experiencing menopause.
- The British Menopause Society - Provides educational resources and guidance on managing menopause.
- Online Communities - Platforms such as Facebook Groups and Reddit forums where women can connect and share experiences.
Menopause: A Natural Part of a Woman’s Life
Menopause is a natural phase of life that comes with its challenges, but understanding the process and exploring treatment options can empower women to manage their symptoms effectively. Whether through conventional methods like HRT or natural alternatives, the key is finding what works best for you but always being aware of the pros and cons of any treatment so you can make an informed decision first.
By adopting a functional medicine viewpoint and heeding the advice of experts like Dr. Lara Briden and Dr. Jolene Brighten, you can approach menopause with confidence and make informed decisions about your health.
For further support and resources, consider connecting with health professionals who specialise in menopausal health and functional medicine. Your transition doesn’t have to be daunting—embrace the change with knowledge and community backing you.
Written by Amy Morris, BSc (Hons) Nutritional Therapy. Amy has been a nutritional therapist for 12 years, specialising in recent years as a functional medicine nutritional therapist. Women’s health, and pre-diabetes and type 2 diabetes prevention are Amy’s specialist areas. Diagnosed with a chronic condition called endometriosis at age 20, this is what motivated Amy to study nutrition. Amy has been in remission for 6 years now, attributing powerful nutrition, lifestyle and bio-identical hormone strategies she now shares with her clients.
Water for Health Ltd began trading in 2007 with the goal of positively affecting the lives of many. We still retain that mission because we believe that proper hydration and nutrition can make a massive difference to people’s health and quality of life. Click here to find out more.
References
1. NHS. (2022, May 17). Menopause. NHS. https://www.nhs.uk/conditions/menopause/
2. Perimenopause: Age, stages, signs, symptoms & treatment. (2021). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/21608-perimenopause
2. Cleveland Clinic. (2021, October 5). Menopause: Age, Stages, Signs, Symptoms & Treatment. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/21841-menopause
3. Cleveland Clinic. (2021, October 5). Menopause: Age, Stages, Signs, Symptoms & Treatment. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/21841-menopause
5. Mayo Clinic. (2023, May 25). Menopause - Symptoms and causes. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/menopause/symptoms-causes/syc-20353397
6. NHS. (2023, July 21). Side effects of hormone replacement therapy (HRT). Nhs.uk. https://www.nhs.uk/medicines/hormone-replacement-therapy-hrt/side-effects-of-hormone-replacement-therapy-hrt/
7. Bioidentical Hormones: Understanding the Basics and Beyond. (2024, June 14). Rupa Health. https://www.rupahealth.com/post/bioidentical-hormones-understanding-the-basics-and-beyond
8. Szmyd, M., Lloyd, V., Hallman, K., Aleck, K., Mladenovik, V., McKee, C., Morse, M., Bedgood, T., & Dinda, S. (2018). The effects of black cohosh on the regulation of estrogen receptor (ERα) and progesterone receptor (PR) in breast cancer cells. Breast Cancer: Targets and Therapy, Volume 10, 1–11. https://doi.org/10.2147/bctt.s144865
9. Beck, V., Rohr, U., & Jungbauer, A. (2005). Phytoestrogens derived from red clover: an alternative to estrogen replacement therapy? The Journal of Steroid Biochemistry and Molecular Biology, 94(5), 499–518. https://doi.org/10.1016/j.jsbmb.2004.12.038
10. Avis, N. E., Coeytaux, R. R., Isom, S., Prevette, K., & Morgan, T. (2016). Acupuncture in Menopause (AIM) study. Menopause, 23(6), 626–637. https://doi.org/10.1097/gme.0000000000000597
11. Woodyard, C. (2011). Exploring the therapeutic effects of yoga and its ability to increase quality of life. International Journal of Yoga, 4(2), 49–54. https://doi.org/10.4103/0973-6131.85485
12.Hoge, E. A., Bui, E., Marques, L., Metcalf, C. A., Morris, L. K., Robinaugh, D. J., Worthington, J. J., Pollack, M. H., & Simon, N. M. (2013). Randomized controlled trial of mindfulness meditation for generalized anxiety disorder. The Journal of Clinical Psychiatry, 74(08), 786–792. https://doi.org/10.4088/jcp.12m08083
13. He, S., Li, H., Yu, Z., Zhang, F., Liang, S., Liu, H., Chen, H., & Lü, M. (2021). The Gut Microbiome and Sex Hormone-Related Diseases. Frontiers in Microbiology, 12. https://doi.org/10.3389/fmicb.2021.711137
14. Sorgen, C. (2006, June 13). Eat Smart for a Healthier Brain. WebMD; WebMD. https://www.webmd.com/diet/features/eat-smart-healthier-brain
14. Ji, J., Jin, W., Liu, S., Zhang, J., & Li, X. (2023). Probiotics, prebiotics, and postbiotics in health and disease. MedComm, 4(6). https://doi.org/10.1002/mco2.420
15. Aziz, T., Hussain, N., Hameed, Z., & Lin, L. (2024). Elucidating the role of diet in maintaining gut health to reduce the risk of obesity, cardiovascular and other age-related inflammatory diseases: recent challenges and future recommendations. Gut Microbes, 16(1). https://doi.org/10.1080/19490976.2023.2297864
16. Schultchen, D., Reichenberger, J., Mittl, T., Weh, T. R. M., Smyth, J. M., Blechert, J., & Pollatos, O. (2019). Bidirectional relationship of stress and affect with physical activity and healthy eating. British Journal of Health Psychology, 24(2), 315–333. https://doi.org/10.1111/bjhp.12355
17. Leproult, R., & Van Cauter, E. (2009). Role of sleep and sleep loss in hormonal release and metabolism. Pediatric Neuroendocrinology, 17(17), 11–21. https://doi.org/10.1159/000262524
18. Ji, M.-X., & Yu, Q. (2015). Primary Osteoporosis in Postmenopausal Women. Chronic Diseases and Translational Medicine, 1(1), 9–13. https://doi.org/10.1016/j.cdtm.2015.02.006
19. Rondanelli, M., Faliva, M. A., Tartara, A., Gasparri, C., Perna, S., Infantino, V., Riva, A., Petrangolini, G., & Peroni, G. (2021). An update on magnesium and bone health. BioMetals, 34(4). https://doi.org/10.1007/s10534-021-00305-0
20. Does Magnesium Help You Sleep? (n.d.). Cleveland Clinic. https://health.clevelandclinic.org/does-magnesium-help-you-sleep
21. National Institutes of Health. (2022). Office of Dietary Supplements - Calcium. Nih.gov. https://ods.od.nih.gov/factsheets/Calcium-HealthProfessional/
22. National Institutes of Health. (2022). Office of Dietary Supplements - Magnesium. National Institutes of Health. https://ods.od.nih.gov/factsheets/Magnesium-HealthProfessional/
23. Voulgaridou, G., Papadopoulou, S. K., Detopoulou, P., Tsoumana, D., Giaginis, C., Kondyli, F. S., Lymperaki, E., & Pritsa, A. (2023). Vitamin D and Calcium in Osteoporosis, and the Role of Bone Turnover Markers: A Narrative Review of Recent Data from RCTs. Diseases (Basel, Switzerland), 11(1), 29. https://doi.org/10.3390/diseases11010029
24.Voulgaridou, G., Papadopoulou, S. K., Detopoulou, P., Tsoumana, D., Giaginis, C., Kondyli, F. S., Lymperaki, E., & Pritsa, A. (2023). Vitamin D and Calcium in Osteoporosis, and the Role of Bone Turnover Markers: A Narrative Review of Recent Data from RCTs. Diseases (Basel, Switzerland), 11(1), 29. https://doi.org/10.3390/diseases11010029
25. Felman, A. (2017, November 28). Vitamin B-12: Functions, deficiency, and sources. Www.medicalnewstoday.com. https://www.medicalnewstoday.com/articles/219822
26. NHS. (2020, August 3). Iron - Vitamins and minerals. NHS; NHS. https://www.nhs.uk/conditions/vitamins-and-minerals/iron/
27. Burgess, L. (2018, January 17). Phytoestrogens: Benefits, risks, and food list. Www.medicalnewstoday.com. https://www.medicalnewstoday.com/articles/320630
28. Bacciottini, L., Falchetti, A., Pampaloni, B., Bartolini, E., Carossino, A. M., & Brandi, M. L. (2007). Phytoestrogens: food or drug? Clinical Cases in Mineral and Bone Metabolism, 4(2), 123–130. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2781234/
29. » How Omega-3 Can Provide Relief for Menopausal Symptoms. (n.d.). Www.menopausecentre.com.au. https://www.menopausecentre.com.au/information-centre/articles/how-omega-3-can-provide-relief-for-menopausal-symptoms/
30. Gunnars, K. (2017). 10 High-Fat Foods That Are Actually Super Healthy. Healthline. https://www.healthline.com/nutrition/10-super-healthy-high-fat-foods
31.How to add more fiber to your diet. (n.d.). Mayo Clinic. https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/fiber/art-20043983#:~:text=Studies%20also%20have%20shown%20that
32. Gunnars, K. (2023, May 3). 22 High-Fiber Foods You Should Eat. Healthline. https://www.healthline.com/nutrition/22-high-fiber-foods
33. Landi, F., Calvani, R., Tosato, M., Martone, A., Ortolani, E., Savera, G., D’Angelo, E., Sisto, A., & Marzetti, E. (2016). Protein Intake and Muscle Health in Old Age: From Biological Plausibility to Clinical Evidence. Nutrients, 8(5), 295. https://doi.org/10.3390/nu8050295
35. Kubala, J. (2022, January 6). 16 Delicious High Protein Foods to Eat. Healthline. https://www.healthline.com/nutrition/high-protein-foods


























Leave a comment