Have you heard of the gut/brain connection? It basically means that your gut health affects your brain health and vice versa.
I have seen this first hand in clinic, where patients come in seeking help for their digestive symptoms (IBS, leaky gut, abdominal pain, diarrhoea, constipation, bloating, heartburn, nausea, the list goes on) and it turns out that they are also dealing with significant anxiety and/or depression.
In this article, we’ll take a closer look at the bidirectional nature of the gut/brain connection, and suggest ways and means of managing both anxiety and depression and, simultaneously, healing the gut.
The Impact of Mental Heath Problems on the Gut
Most of us know what it’s like to feel emotional about something, be it frustration, anger, stress, sadness or anxiety; we lose our appetite, feel sick, have butterflies in our stomach or get the runs.
How we feel mentally can have a direct impact on our gut, and this can be short-lived, or if those feelings become chronic, the gut symptoms can become chronic too.
One study showed chronic stress to be a significant predictor of gastrointestinal disorders in 668 students, and researchers surmised that stress-reducing interventions could be beneficial for these patients.
If you suffer from long-term digestive issues, this can directly influence how you feel too, and you may start to experience mood changes, anxiety or depression.
You may also encounter other brain symptoms such as lack of focus and concentration, memory issues and foggy thinking.
This connection between the gut and the brain has received increased attention over the last few years, with research gathering momentum in a bid to find alternative treatments for depression, amongst other things.
Psychological Therapies for Gastrointestinal Symptoms
Some research supports the use of psychological approaches for improving digestive issues.
According to Harvard Medical School, evidence suggests that methods including cognitive behavioural therapy, hypnosis and relaxation therapies such muscle relaxation, positive visualisation and soothing music can all help to significantly improve severe GI symptoms.
Some trials also support the use of mindfulness and meditation for improving IBS symptoms and easing anxiety and depression.
One study published by the American Journal of Gastroenterology found that a mixture of daily mindfulness (a combination of reading of self-help books, meditation and mindful yoga) improved IBS symptoms, anxiety, psychological distress and the quality of life in women with IBS.
The treatment lasted eight weeks, with a follow-up three months after the trial concluded.
Interestingly, these patients benefited from continuous improvement at the three-month mark, suggesting that mindfulness practice has long-lasting effects.
Serotonin Lives in Your Gut and Your Brain
It is commonly believed that low serotonin in the brain is linked to low mood and depression (although opinions are changing on this). But did you know that there is more serotonin in your gut than in your brain?
Serotonin helps with gut motility, meaning it speeds up digestion and helps with the expulsion of waste. So if you have food poisoning, the serotonin in your gut will encourage the toxins to rapidly leave your intestines.
While more research is needed, it is now thought that due to the gut-brain axis, digestive serotonin may also have an impact on mood.
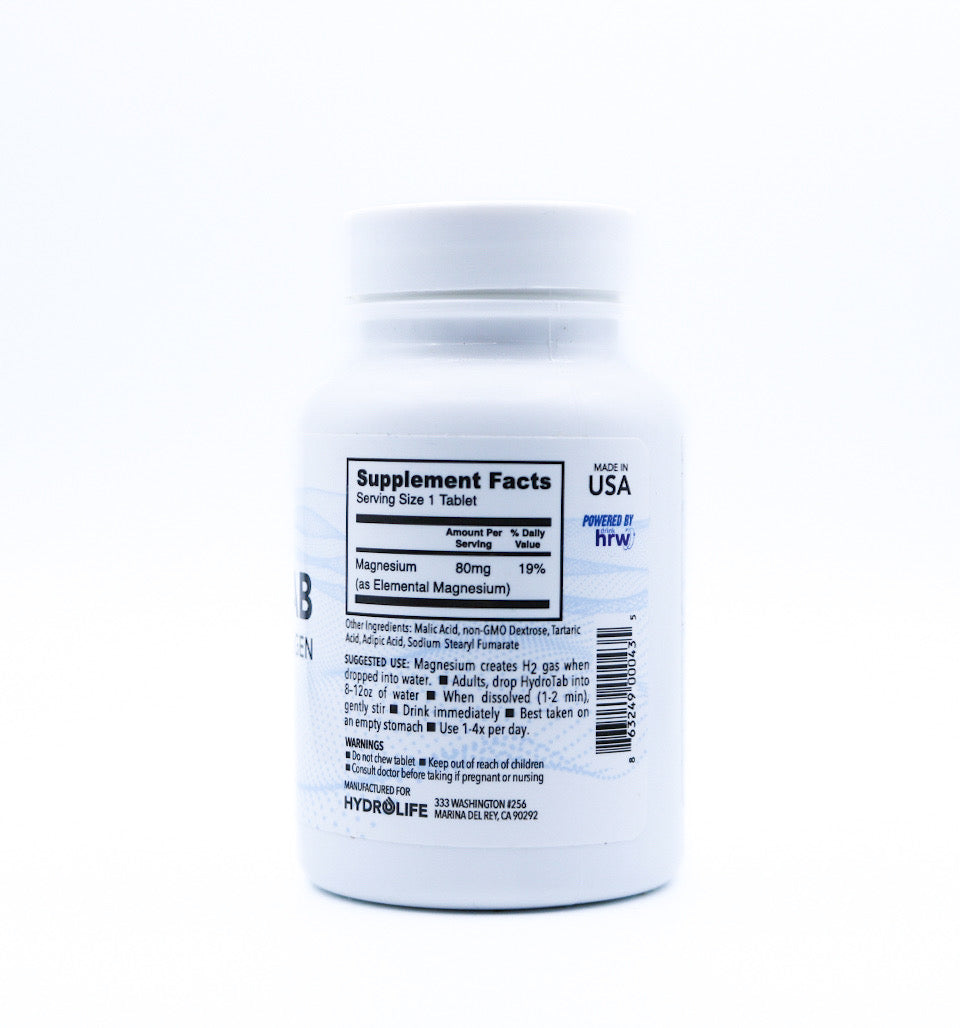
Tryptophan is an amino acid that increases serotonin, and some research supports increased consumption with improved mood.
One way that you can increase your serotonin levels is to eat foods high in tryptophan such as bananas, turkey, chicken, tuna, halibut and salmon, shellfish, lean red meat, eggs, non-GMO soy, nuts and seeds – particularly pumpkin seeds and oats.
Probiotics for Stress, Anxiety and Depression
Over 70% of your immune system lives in your gut, and this is down to its diverse microbiota (gut flora) consisting of trillions of microorganisms including over 1,000 different species of gut bacteria, as well as fungi and viruses.
These all co-habit in an intelligent and delicate balance to keep us healthy and robust.
Our gut lining is also a protective barrier, preventing any toxins, harmful substances, bacteria and food waste from leaking into our bloodstream.
Many believe that leaky gut and dysbiosis (microbial imbalance of the gut) is due to exposure to chronic disease, viruses, medications such as antibiotics and NSAIDs, and stress.
Compromised gut health and leaky gut can both lead to inflammation which is now commonly believed to underlie chronic diseases such as type 2 diabetes, cardiovascular disease, rheumatoid arthritis and other autoimmune diseases.
It may also contribute to depression, anxiety and common mental disorders. And some researchers have found that depressed patients with higher inflammatory markers are less likely to respond to antidepressants and more likely to benefit from taking anti-inflammatory medication.
Probiotics have been shown to reduce inflammation in the gut, and researchers acknowledge the link between probiotics, brain development and behaviour. Indeed, several positive studies link them to improved brain chemistry and mental health.
Probiotics help to aid nutrient absorption and blood sugar balance, improving anxiety and depressive symptoms.
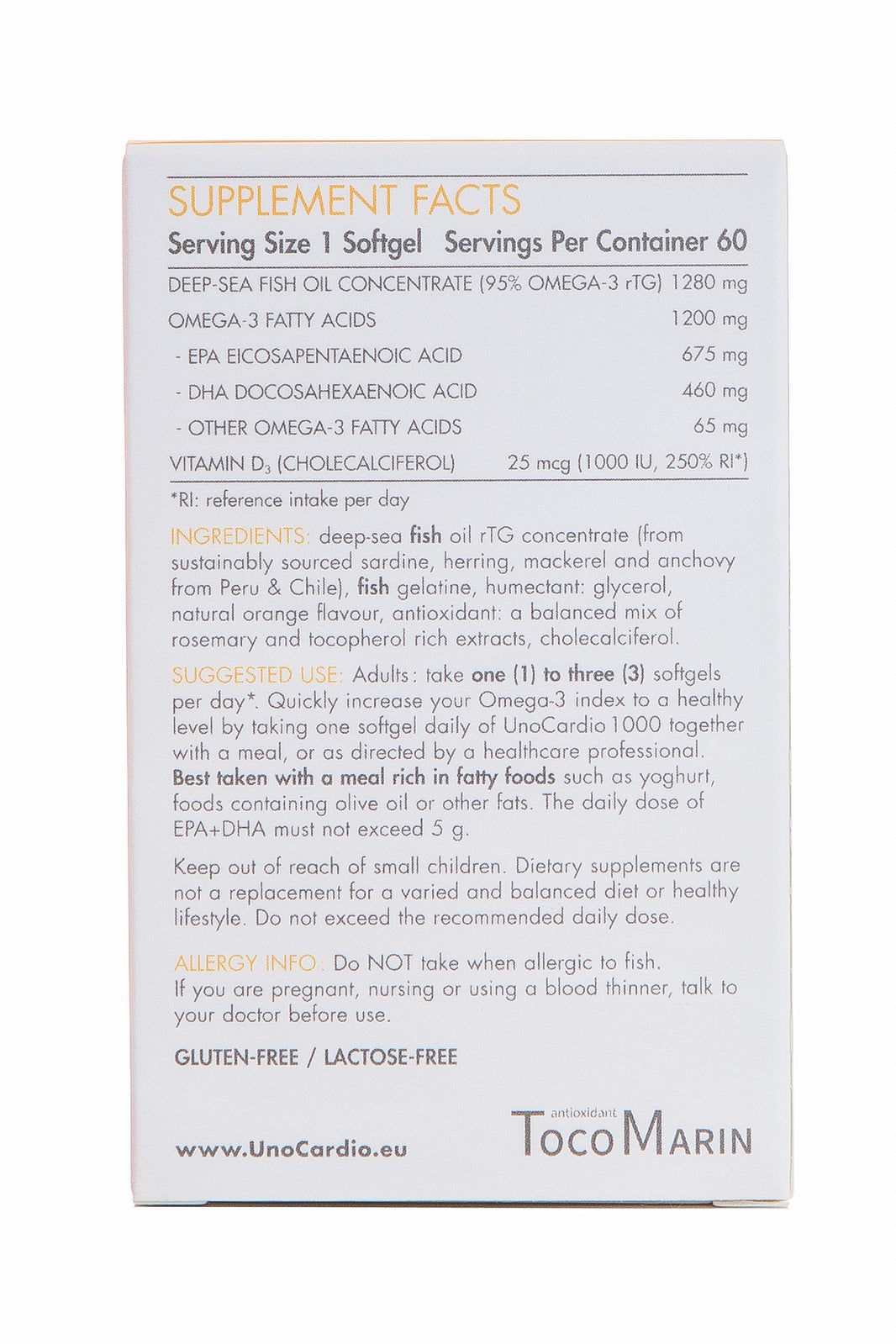
If sufficiently high-quality, they can improve the symptoms of IBS, and in one 2017 study depression and quality of life improved in 64% of IBS patients six weeks after taking the probiotic Bifidobacterium longum NCC3001.
Probiotics may also have a neuroprotective role, modulating the stress response.
In one trial on random volunteers, the more depressed the patients, the happier they felt after taking probiotics for three weeks.
In participants who were generally of ‘good mood’, probiotics improved constipation and left them feeling more clear-headed, confident and elated.
Probiotics have also been shown to improve cortisol levels, reduce depressive symptoms and lower the stress response as efficiently as those taking Diazepam or Citalopram (commonly prescribed anti-anxiety and antidepressant medications).
Conclusion
The take-home? A healthy gut means a healthy mind – and vice versa.
The discovery of the gut-brain axis has highlighted the importance of gut health, not only for a fully functioning digestive system but also for good mental and emotional wellbeing.
Practices such as mindfulness, meditation, yoga, walking in nature and feeling gratitude can all help to improve gastrointestinal symptoms, mental outlook and mood.
Taking probiotics may help to reduce depression symptoms and feelings of anxiety while strengthening gut integrity and reducing overall inflammation (a contributing factor to mental disorders).
Another way you can look after your gut, increase serotonin levels and modulate your mood is to eat plenty of tryptophan foods while adding raw fermented foods such as sauerkraut and kimchi to your daily diet.
Ensure you’re eating plenty of fibre as well as prebiotic foods like under-ripe bananas, apples, oats, onions, garlic and leeks. Consuming these as part of a natural, whole-food diet will go a long way to keeping your gut and mind healthy.
To find out more about our premium range of Progurt probiotics, click here.
Written by Rebecca Rychlik, Nutritional Therapist and Homeopath. Follow Rebecca on Instagram, Facebook and Medium, @rebeccabitesback.























Leave a comment