Living with migraines can be an unpredictable and distressing experience. These intense headaches are often accompanied by sensory disturbances known as auras, extreme aversion to light and sound, and occasionally, nausea. For many, migraines are chronic and can disrupt daily life, making understanding and managing them a top priority. In this comprehensive guide, we’ll explore the diverse types of migraines and provide insights into how diet and lifestyle changes – including supplements – can offer much-needed relief.
Migraine Types
Migraines are not a one-size-fits-all affliction. They come in various forms, each with its own set of symptoms and triggers. Classifications often depend on whether they occur with an aura or without, but other features like frequency and duration also play a role. Here are several types you should be familiar with:
1. Migraine without Aura
This is the most common type of migraine. It involves moderate to severe pounding or pulsing pain, which is typically felt on one side of the head. Other symptoms can include nausea, vomiting, and sensitivity to light and sound.
2. Migraine with Aura
Migraines with aura are characterised by the development of neurological symptoms – most commonly visual disturbances – before the headache begins. These auras can include flashes of light, blind spots, or difficulty speaking.
3. Chronic Migraine
A chronic migraine occurs when migraines happen on 15 or more days a month for over three months, with at least eight days having migraine-like symptoms. It’s often the case that they start as episodic migraines and become chronic over time.
4. Vestibular Migraine
Vestibular migraines are associated with vertigo and imbalance. Attacks can occur with or without the typical migraine headache but must occur with other migraine symptoms at least half the time.
5. Hemiplegic Migraine
People with hemiplegic migraines may experience temporary paralysis on one side of the body (hemiplegia) as a symptom. This condition can be particularly frightening but symptoms typically resolve within 24 hours.
6. Menstrual Migraine
As the name suggests, menstrual migraines are associated with a woman’s menstrual cycle. They typically occur around the time of menstruation and may be more severe and less responsive to treatment than migraines not associated with a woman's cycle.
Each of these types of migraines can be managed uniquely, and understanding which type you experience is crucial for developing an individualised treatment plan.
Preventative Measures
Lifestyle changes can significantly impact the frequency and severity of migraines. Here are some preventive measures that have shown promise:

Stay Hydrated
Dehydration is a known trigger for migraines (1). Keeping well-hydrated can help prevent attacks. However, not all fluids are created equal; caffeinated drinks and alcohol, for example, can also trigger migraines in some individuals.
Get Adequate Sleep
Changes in your sleep pattern, like getting too little or too much sleep, can trigger migraines (2). Establishing a regular sleep schedule and ensuring you get the recommended seven to eight hours of sleep each night can be beneficial.
Identify and Avoid Triggers
Common migraine triggers include certain foods (e.g., aged cheeses, chocolate), intense physical activity, stress, and hormonal changes (3). Keeping a detailed migraine journal can help identify personal triggers that can be avoided.
Manage Stress
Stress is a major trigger for many migraine sufferers (4). Techniques such as relaxation, meditation, or Cognitive Behavioral Therapy (CBT) can be used to manage stress and reduce the frequency of migraines.
Regular Exercise
Engaging in regular, moderate exercise can reduce the frequency and intensity of migraines (5). However, sudden, intense physical activity can act as a trigger, so it’s important to find a balance.
Maintain a Healthy Weight
Obesity is a risk factor for migraines, particularly in females (6). For those who are overweight, even a modest reduction can reduce the frequency of attacks.
Balanced Eating Patterns
Skipping meals or fasting can trigger migraines in some individuals (7). Maintaining a regular eating schedule with balanced nutritional intake is essential. High-protein, low-carb, and low-fat diets have all shown benefits for migraine prevention in different individuals.
While these measures can be effective for many, some may find that additional support from supplements and specific dietary protocols can make a remarkable difference.
Supplements for Migraines
Dietary supplements can provide an additional layer of support for those managing migraines. While it's important to consult a healthcare professional before starting any new supplement regimen, here are several that have demonstrated potential for migraine management:

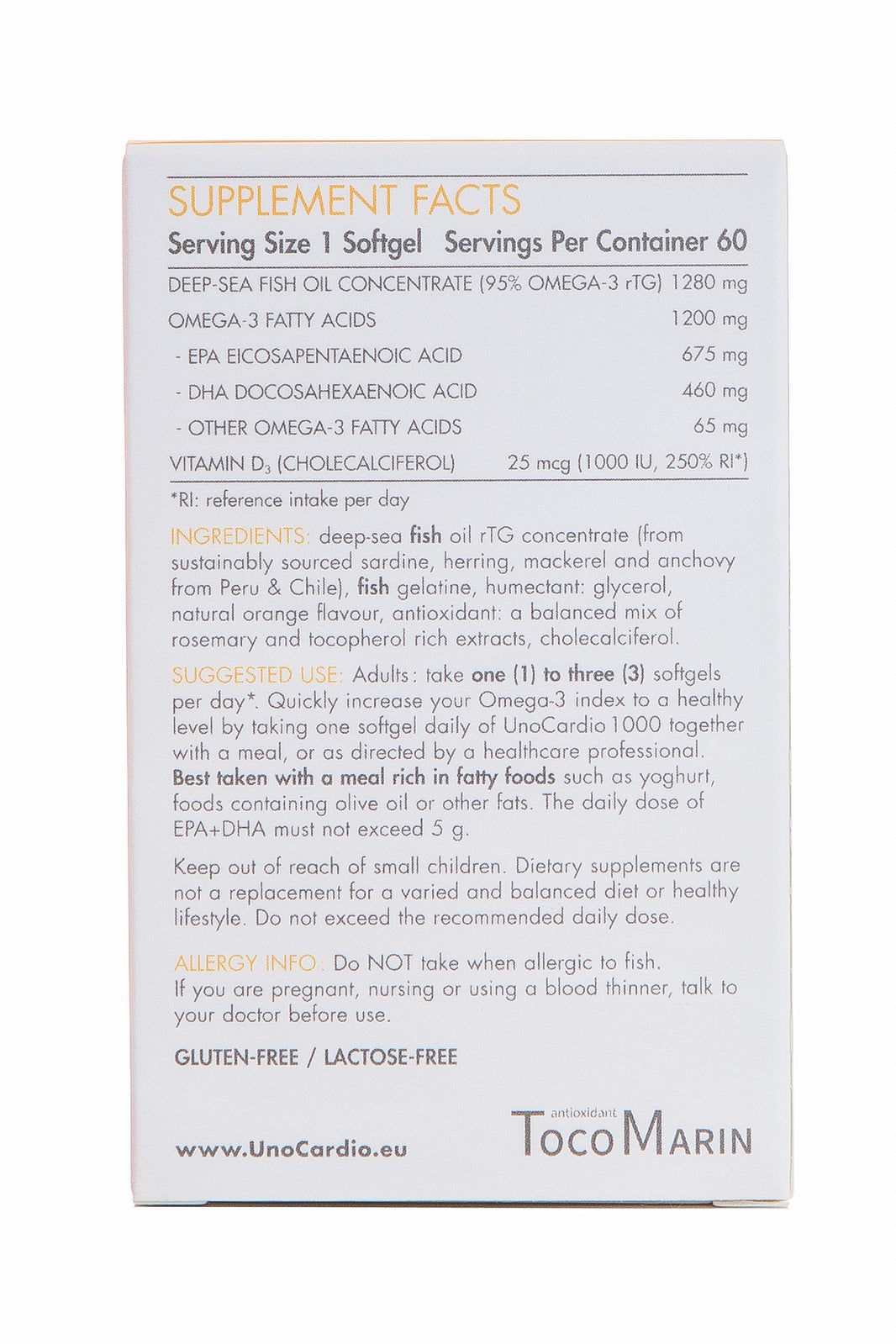
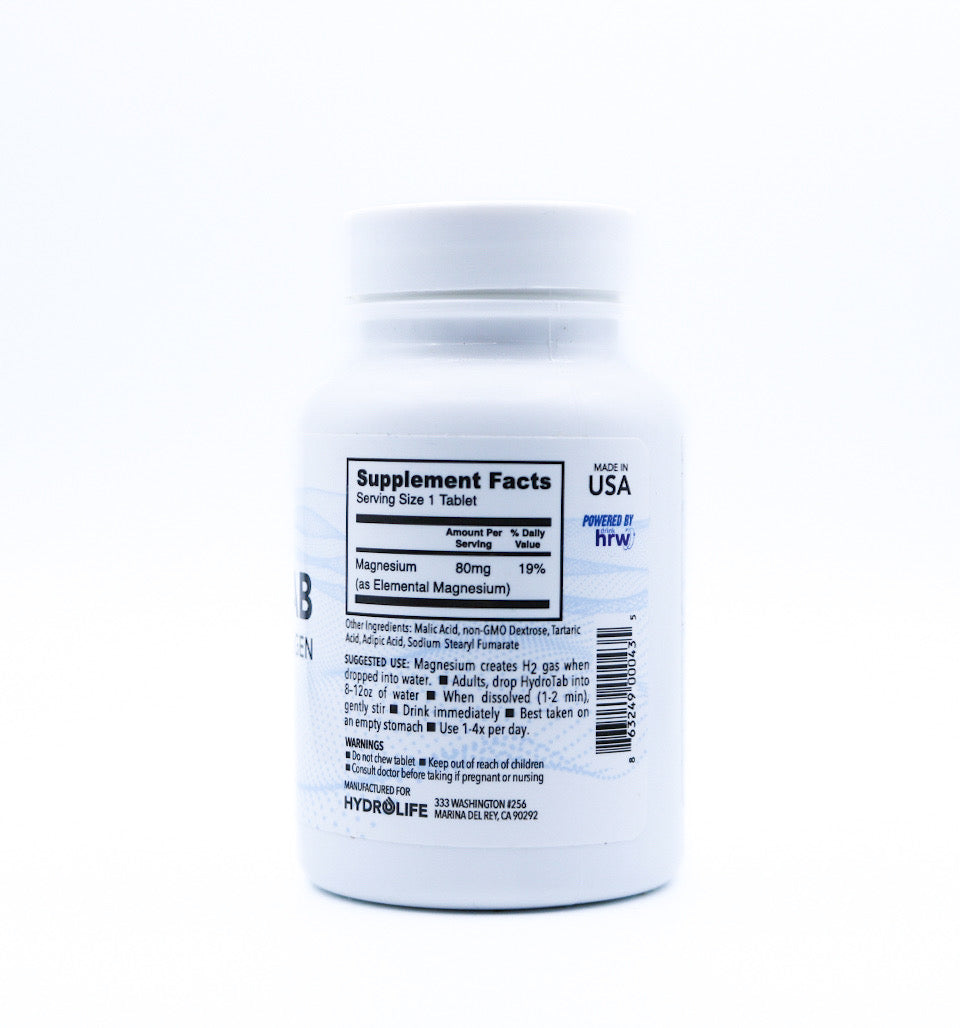
1. Magnesium
Many migraine sufferers have lower than normal levels of magnesium (8). Supplementing with magnesium has been found to reduce the frequency of migraines, particularly for those with a magnesium deficiency. A recommended dose is about 400 to 500 mg daily.
2. Coenzyme Q10
Coenzyme Q10 is an antioxidant that occurs naturally in the body and is involved with the production of energy within cells. Several studies have suggested that CoQ10 may reduce the frequency of migraines (9).
3. Riboflavin (Vitamin B2)
Riboflavin is a B vitamin found in food and used as a dietary supplement. Some evidence suggests it may help prevent migraines, particularly in cases where patients have specific genetic variants believed to be linked to migraines (10).
4. Butterbur
Butterbur is a plant extract that has been used traditionally to treat headaches. Some clinical trials have suggested that supplements of butterbur may reduce the frequency of migraines, potentially by reducing inflammation (11).
Supplements should be used in conjunction with a balanced diet and lifestyle changes, as they are not a substitute for a healthful foundation. It’s essential to source your supplements from reputable brands that ensure quality and purity.
Dietary Management of Migraines
Your diet can play a significant role in migraine management. Certain foods and nutrients may act as triggers, while others can provide protection against migraines. Here are some strategies to consider when adjusting your diet to help manage your migraines:
Identify Trigger Foods
While triggers can be highly individual, some common dietary culprits include alcohol, caffeine, aged cheeses, preserved meats, and foods that contain MSG. In your journal, note any dietary patterns or specific items that tend to precede a migraine.
Ensure Regular and Balanced Meals
Skipping meals can lead to low blood sugar, which is a common migraine trigger. Eating balanced meals with a mix of healthy fats, lean proteins, and complex carbohydrates can help to maintain stable blood sugar levels.
Eat a Whole Food Diet
A diet rich in whole foods, including plenty of fruits, vegetables, whole grains, and lean proteins, can provide the nutrients necessary for overall health and may reduce the frequency of migraines.
Hydrate with Water
Staying hydrated is important for overall health and can be particularly beneficial for migraine prevention.
Consider a Low Tyramine Diet
Tyramine is a compound found in foods that can trigger migraines. It is formed from the breakdown of certain proteins in foods that have been aged, fermented, or stored for a long time. A low-tyramine diet may be beneficial for some migraine sufferers.
Adopt an Anti-Inflammatory Diet

Chronic inflammation has been linked to migraines (12). An anti-inflammatory diet, which includes foods like fatty fish, flaxseeds, and dark leafy greens, may help reduce the frequency and severity of migraines.
Your dietary approach should be tailored to your individual needs, and it's important to work with a healthcare professional or dietitian to ensure that your diet supports your health and well-being.
Lifestyle Adjustments for Migraine Management
In addition to diet and supplements, several lifestyle adjustments can support your efforts to manage migraines effectively:
Effectively Manage Technology
Overexposure to screens, especially those with high brightness and blue light, can trigger migraines. Implement screen-time breaks and use blue-light filtering technology to minimise this risk.
Manage Your Environment
Sensory stimuli such as intense or flickering lights, loud noises, and strong odours can trigger migraines. Modify your surroundings to reduce exposure to these triggers.
Tackle Hormonal Migraines
Hormonal fluctuations, particularly for women, can play a role in migraines. Hormonal treatment and contraceptives can help reduce the severity and frequency of hormonal migraines.
Keep a Consistent Routine
Maintaining a consistent routine for sleeping, eating, and daily activities can help stabilise your body's rhythms and reduce the risk of migraine onset.
Seek Adequate Support
Living with migraines can be challenging and isolating. Seek support from friends, family, or a professional who can offer understanding and guidance.
The Journey to Better Migraine Management
Migraine management is an ongoing process of discovery and adaptation. Understanding the different types of migraines, including their triggers and symptoms, is the first step towards creating a personalised and effective management plan. By incorporating dietary changes, supplements, and other supportive lifestyle modifications, you can significantly reduce the impact of migraines on your life.
It's important to approach migraine management holistically and to be patient with the process. Small changes can add up to significant results over time. Always work with a healthcare professional to ensure that your approach is safe and suitable for your individual needs.
Migraine management may sometimes feel like trial and error, but with the right knowledge and support, you can reduce the frequency and severity of your attacks and regain a greater quality of life. Remember, you are not alone in this – there is a wealth of resources and communities available to help you on your journey.
Written by Amy Morris, BSc (Hons) Nutritional Therapy. Amy has been a nutritional therapist for 12 years, specialising in recent years as a functional medicine nutritional therapist. Women’s health, and pre-diabetes and type 2 diabetes prevention are Amy’s specialist areas. Diagnosed with a chronic condition called endometriosis at age 20, this is what motivated Amy to study nutrition. Amy has been in remission for 6 years now, attributing powerful nutrition, lifestyle and bio-identical hormone strategies she now shares with her clients. https://www.greathealthnaturally.co.uk/
Water for Health Ltd began trading in 2007 with the goal of positively affecting the lives of many. We still retain that mission because we believe that proper hydration and nutrition can make a massive difference to people’s health and quality of life. Click here to find out more.
References
1) Nelson, J. (n.d.). The Link Between Migraine and Dehydration. WebMD. https://www.webmd.com/migraines-headaches/migraine-dehydration-link
2) Ahn, A. H., & Goadsby, P. J. (2013). Migraine and sleep: new connections. Cerebrum : the Dana forum on brain science, 2013, 15.
3) Diet and Headache Control. (n.d.). American Migraine Foundation. https://americanmigrainefoundation.org/resource-library/diet/
4) Maleki, N., Becerra, L., & Borsook, D. (2012). Migraine: maladaptive brain responses to stress. Headache, 52 Suppl 2(Suppl 2), 102–106. https://doi.org/10.1111/j.1526-4610.2012.02241.x
5) Ahn A. H. (2013). Why does increased exercise decrease migraine?. Current pain and headache reports, 17(12), 379. https://doi.org/10.1007/s11916-013-0379-y
6) Bond, D. S., Roth, J., Nash, J. M., & Wing, R. R. (2011). Migraine and obesity: epidemiology, possible mechanisms and the potential role of weight loss treatment. Obesity reviews : an official journal of the International Association for the Study of Obesity, 12(5), e362–e371. https://doi.org/10.1111/j.1467-789X.2010.00791.x
7) Turner, D. P., Smitherman, T. A., Penzien, D. B., Porter, J. A., Martin, V. T., & Houle, T. T. (2014). Nighttime snacking, stress, and migraine activity. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia, 21(4), 638–643. https://doi.org/10.1016/j.jocn.2013.08.013
8) Mauskop, A., & Varughese, J. (2012). Why all migraine patients should be treated with magnesium. Journal of neural transmission (Vienna, Austria : 1996), 119(5), 575–579. https://doi.org/10.1007/s00702-012-0790-2
9) Efficacy of coenzyme Q10 for the prevention of migraine in women: A randomized, double-blind, placebo-controlled study. (2017). European Journal of Integrative Medicine, 16, 8–14. https://doi.org/10.1016/j.eujim.2017.10.003
10) Nematgorgani, S., Razeghi-Jahromi, S., Jafari, E., Togha, M., Rafiee, P., Ghorbani, Z., Ahmadi, Z. S., & Baigi, V. (2022). B vitamins and their combination could reduce migraine headaches: A randomized double-blind controlled trial. Current journal of neurology, 21(2), 105–118. https://doi.org/10.18502/cjn.v21i2.10494
11) Silberstein, S. D. (2010, January 1). Chapter 27 - Migraine: preventive treatment (M. J. Aminoff, F. Boller, & D. F. Swaab, Eds.). ScienceDirect; Elsevier. https://www.sciencedirect.com/science/article/abs/pii/S0072975210970279
12) Kursun, O., Yemisci, M., van den Maagdenberg, A. M. J. M., & Karatas, H. (2021). Migraine and neuroinflammation: the inflammasome perspective. The Journal of Headache and Pain, 22(1). https://doi.org/10.1186/s10194-021-01271-1

























Leave a comment