The hormone insulin is a key player in the maintenance of optimal health through the regulation of glucose in the body. Without insulin, the body is unable to use or store the glucose for energy, resulting in damage to the organs and the blood vessels.
High blood sugar can cause many complications such as nerve damage, eye problems, heart disease, stroke, kidney problems, and foot damage. These are just a few examples. The lack of insulin, or resistance to insulin, can also lead to the development of Type II diabetes. And no, it's not just because you ate too much sugar... Although dietary factors, being overweight and lack of physical activity can all play a role in the development of diabetes, but they're not the only factors involved.
Considering the negative ramifications from an imbalance in insulin levels, it is important that people understand the necessity to make dietary and lifestyle changes to ensure the body remains healthy, thus maintaining a good insulin balance. This is not only for diabetics or pre-diabetics, but for anyone who values their health and well-being.
What is insulin?
Insulin is a hormone made by the pancreas and allows your body to use sugar (glucose) from carbohydrates in the food that you eat for energy or to store glucose for future use (1). Insulin helps to lower the amount of sugar in your bloodstream, and can be seen as the “protector” of blood sugar levels. This is why having a fasting glucose test alone will not definitively tell you if you have pre-diabetes or full blown type 2 diabetes.
Insulin has several effects on the body. During digestion in the small intestine, carbohydrates, proteins, and fats are broken down into simpler forms:
- Carbohydrates are converted into sugars, primarily glucose, by carbohydrase enzymes found in the mouth, stomach, and small intestine.
- Proteins are digested into amino acids in the stomach and small intestine and only a small amount of glucose.
- Fats are broken down into fatty acids and glycerol by lipase enzymes in the intestine and only a small amount of glucose.
This rising blood glucose level from the glucose that came in large amounts from the digested carbohydrates, is detected by the pancreas and triggers the release of insulin. Insulin is then produced and then helps glucose to enter cells from the bloodstream (2). In muscle and fat cells, stored glucose (glycogen) is used for energy, and in fat cells, glucose is converted into fat to be used for energy at a later date (3). In the liver, insulin promotes the storage of glucose and the production of fat. When insulin is not present, the opposite happens: muscle and fat cells use stored glucose and do not take up more glucose from the bloodstream, fat in the form of fatty acids is released from fat cells, and glucose and fat production is increased in the liver. This process ensures that a minimum amount of glucose is used as energy and the maximum amount is stored.
Type 1 diabetes is an autoimmune disease and it can strike regardless of age, gender, or race (4). If you have Type 1 diabetes, you will require insulin therapy for the rest of your life. Type 2 diabetes is often associated with being overweight or having a family history of diabetes. This is because carrying excess body fat, particularly around the abdomen, increases the likelihood of insulin resistance and Type 2 diabetes. More than 90 percent of people with diabetes have Type 2 diabetes, which usually begins in adulthood (5). However, not everyone with type 2 diabetes is overweight (6).
The Role of Insulin in The Body
This is where we really start to see the importance of understanding the hormone insulin. As we know, it regulates the levels of glucose in the blood. When we eat, a rush of sugar or glucose is released into the blood and is toxic to our bodies, so insulin is released from the pancreas to store this fuel for future use. The sugar is stored in the liver and muscle in a form called glycogen.
Once these stores are full, the sugar is stored as fat (7). Something that is all too common in today's society with an abundance of food, and an overreliance on processed carbohydrates; the main source of glucose. Here lies an important point. With the absence of insulin, glucose can't enter the cells and is left circulating in the blood. High blood glucose is known as hyperglycemia and is a bad thing due to the damage caused to the blood vessels and is the primary cause of the complications that we see in diabetics.
By making healthy lifestyle choices, however, it is possible to avoid the damage caused by high blood glucose and prevent type 2 diabetes from developing. This is, of course, easier to understand if we have an idea of what high and low is in terms of blood glucose.
Testing Glucose and Insulin: What the Levels Mean

Regular glucose testing is crucial for monitoring blood sugar levels, especially for individuals with diabetes or those at risk. However, it’s equally important to test insulin levels alongside glucose. Insulin is the hormone responsible for regulating blood sugar by facilitating the uptake of glucose into cells, thus acting as the protector of glucose levels.
Both glucose and insulin tests are typically conducted in a fasted state to ensure accurate results. The standard range for fasting blood glucose levels is generally between 70–99 mg/dL (3.9–5.5 mmol/L (8), while for insulin, the standard fasting range is between 2–25 µIU/mL (9).
On the other hand, functional medicine practitioners often use narrower reference ranges to identify potential issues earlier. For example, they consider optimal fasting glucose levels to be between 75–86 mg/dL (4.1–4.8 mmol/L) (10)and fasting insulin levels to be between 2–5 µIU/mL(10). This approach can offer a more proactive stance in managing and preventing metabolic conditions.
By regularly testing both glucose and insulin levels, you can gain a comprehensive understanding of your metabolic health. Adopting the functional medicine approach may offer more precise guidance on maintaining optimal health and preventing chronic conditions related to blood sugar regulation.
The Importance of Maintaining Insulin Balance; Cancer Cells, Weight Gain-Hunger Loop and Blood Sugar Balance.
Simply put, attaining and maintaining a state of optimal nutrition can be a constant balancing act. A multitude of interconnected factors contribute to wellness, and it is easy to underestimate the effect of even the tiniest imbalance.
Blood sugar regulation is a good example; it has long been known that imbalanced or high and low blood sugar is a primary symptom of poor health, diabetes, and a vast number of related obesity and cardiovascular diseases. What may be less known is that the hormone primarily responsible for reducing blood sugar is also one of nature's most powerful growth factors. This dual role as a blood sugar regulator and potent anabolic agent is insulin's key to understanding the importance of maintaining blood sugar in healthy ranges. Insulin's ability to increase the growth of cells (both healthy and cancerous) and its potential to promote weight gain are two undesirable effects of the hormone if blood sugar is not properly regulated (11).
During times of high blood sugar (or energy abundance), the increased insulin is essentially a signal for cells to grow and divide, and it increases uptake of many substrates including ions, amino acids, and carbohydrates to further cell growth. This effect on cell growth is why diabetics have an increased rate of retinopathy, nephropathy, and neuropathy and is also why having constantly high insulin can accelerate the growth of tumours and increase the risk of certain inflammatory diseases. High insulin is also a major promoter of weight gain. This is because insulin's promotion of all these growth effects will occur to the extent that less energy in the form of blood glucose and fats will be available for use by the body. This decrease in energy availability is what can ultimately lead to hunger, fatigue, and decreased physical activity. To store more energy for a time when it is needed and thus avoid a potential energy crisis in the cell, the obvious and natural choice is to eat more. However, excess energy will only serve to further elevate blood sugar and increase the anabolic effects of insulin.
Insulin Resistance and its Consequences
Whether pre- or type 2 diabetes develops, the onset is characterised by progressively worsening insulin resistance. Insulin resistance is a major factor in the metabolic syndrome, which is defined as clinical and physiological disorders in patients including obesity, immoderate levels of blood fats, hypertension, and a greater risk in developing cardiovascular disease.
The metabolic syndrome is also closely associated with Polycystic Ovary Syndrome (PCOS), which affects women. Other issues that insulin resistance can lead to include elevated levels of uric acid and gout.
Insulin resistance is the underlying issue in type 2 diabetes and has been shown to affect the function and production of nitric oxide (NO) (12). This molecule is critical in the regulation of blood flow and the prevention of narrowing of the blood vessels. During insulin resistance, the effects of insulin on NO are diminished and can be attributed to various vasculopathies (diseases of the blood vessels) frequently seen in diabetes.
High cholesterol and coronary artery disease have been linked with insulin resistance due to less effective response on the LDL cholesterol receptors, leading to higher levels of damaging LDL cholesterol.
Insulin resistance is actually not a clearly defined physiological disorder state and is generally classed by a reduced ability of specific tissues (skeletal muscle, adipose tissue, and the liver) to respond to normal or increased levels of insulin in glucose uptake and storage process. The method by which insulin increases glucose uptake has been the result of extensive research, where insulin promotes the translocation of GLUT4 glucose transporters to be positioned on the cell membrane from their internal storage sites. The significance of this is seen in muscle cells.
Normally the largest site in the body for glucose uptake and disposal, a decrease in insulin action modifies the GLUT4 in myocytes and affects the ability for glucose to move into the cells. This has a large impact on competitive sports performance and recovery for athletes who may be unknowingly losing efficiency in glucose utilisation.
Adopt the Glucose Goddess’s Eating Strategies to Keep Insulin in Check

In the fight against type 2 diabetes and prediabetes, adopting the Glucose Goddess's eating strategies can be a game changer. By starting each meal with a fibre-rich green starter, such as asparagus, broccoli, or a simple spinach salad, you can significantly slow down the digestion process (13). This leads to more stable blood sugar levels and a prolonged sense of fullness, which is crucial for weight management. Maintaining a healthy weight is one of the key factors in reducing the risk of developing type 2 diabetes. Additionally, the fiber in these greens helps to prevent the rapid spikes in blood glucose that can damage insulin sensitivity over time.
Another effective strategy is to consume a tablespoon of vinegar, preferably apple cider vinegar, diluted in water before meals. Research shows that vinegar can improve insulin sensitivity, making it easier for cells to absorb glucose from the blood (14). This small habit can have a substantial impact on preventing insulin resistance, a precursor to both prediabetes and type 2 diabetes. For those who find drinking vinegar unpalatable, incorporating it into a salad dressing can offer similar benefits.
Starting your day with a savory, high-protein breakfast is another critical tip from the Glucose Goddess. Foods like eggs, Greek yogurt, tofu, and lean meats can help regulate blood sugar levels throughout the day (15). Unlike sugary breakfasts that cause a rapid spike and subsequent crash in blood glucose, savory breakfasts provide sustained energy and help keep glucose levels stable. Stabilizing morning glucose levels sets a positive tone for the rest of the day, reducing the likelihood of insulin resistance and the development of type 2 diabetes.
Finally, incorporating post-meal movement into your daily routine can further enhance blood glucose management (16). Activities like a 10 to 20-minute walk, some light yoga, or a quick set of squats can significantly reduce postprandial blood sugar levels. This is because physical activity promotes glucose uptake by muscles, improving overall insulin sensitivity and helping to maintain stable blood sugar levels. By integrating these research-backed strategies into daily life, individuals can effectively manage their blood glucose levels, thereby reducing the risk of developing type 2 diabetes and prediabetes.
Enhancing Longevity Through Insulin Optimisation
A strong desire to not only extend life but to truly thrive in our later years is a common sentiment expressed in patients visiting wellness professionals irrespective of their current age. A powerful methodology towards achieving this goal is fundamental for considering that it is the quality of years lived that is so greatly feared to be lost in the face of ever-increasing lifespan.
The good news is that by its profound influence on healthspan, insulin presents a robust and valid target towards enhancing the quality and not just the quantity of life. Nothing is more certain in the field of ageing and longevity than the role of insulin and insulin signalling.
High insulin levels accelerate the abnormalities and weaken the ability of cells to survive and function properly. Over many years, detrimental effects are distributed to all tissues and in particular to those most relevant to the quality of life in later years (brain, cardiovascular system). Theoretically if one were to compile a list of all the internal or external sabotaging factors reducing the human health span, the result would be akin to a list of situations provoking insulin resistance. A great next step with this knowledge is to test your insulin levels with an experienced health practitioner such as one who specialises in functional medicine, and to eat in a way that reduces big insulin and glucose spikes. They can also guide you with other tests that can be carried out at the same time or after based on the results, helping understand your whole health picture and not just one isolated test. However, in saying that, insulin is rarely tested in the UK and its importance should be that even testing in isolation, knowing insulin levels alone can reveal a lot - more so than just a standard blood sugar test which frequently misses pre-diabetes - the first stage before type 2 diabetes that a person can sit in for 8-10 years undiagnosed due to not testing insulin
Written by Amy Morris, BSc (Hons) Nutritional Therapy. Amy has been a nutritional therapist for 12 years, specialising in recent years as a functional medicine nutritional therapist. Women’s health, and pre-diabetes and type 2 diabetes prevention are Amy’s specialist areas. Diagnosed with a chronic condition called endometriosis at age 20, this is what motivated Amy to study nutrition. Amy has been in remission for 6 years now, attributing powerful nutrition, lifestyle and bio-identical hormone strategies she now shares with her clients.
Water for Health Ltd began trading in 2007 with the goal of positively affecting the lives of many. We still retain that mission because we believe that proper hydration and nutrition can make a massive difference to people’s health and quality of life. Click here to find out more.
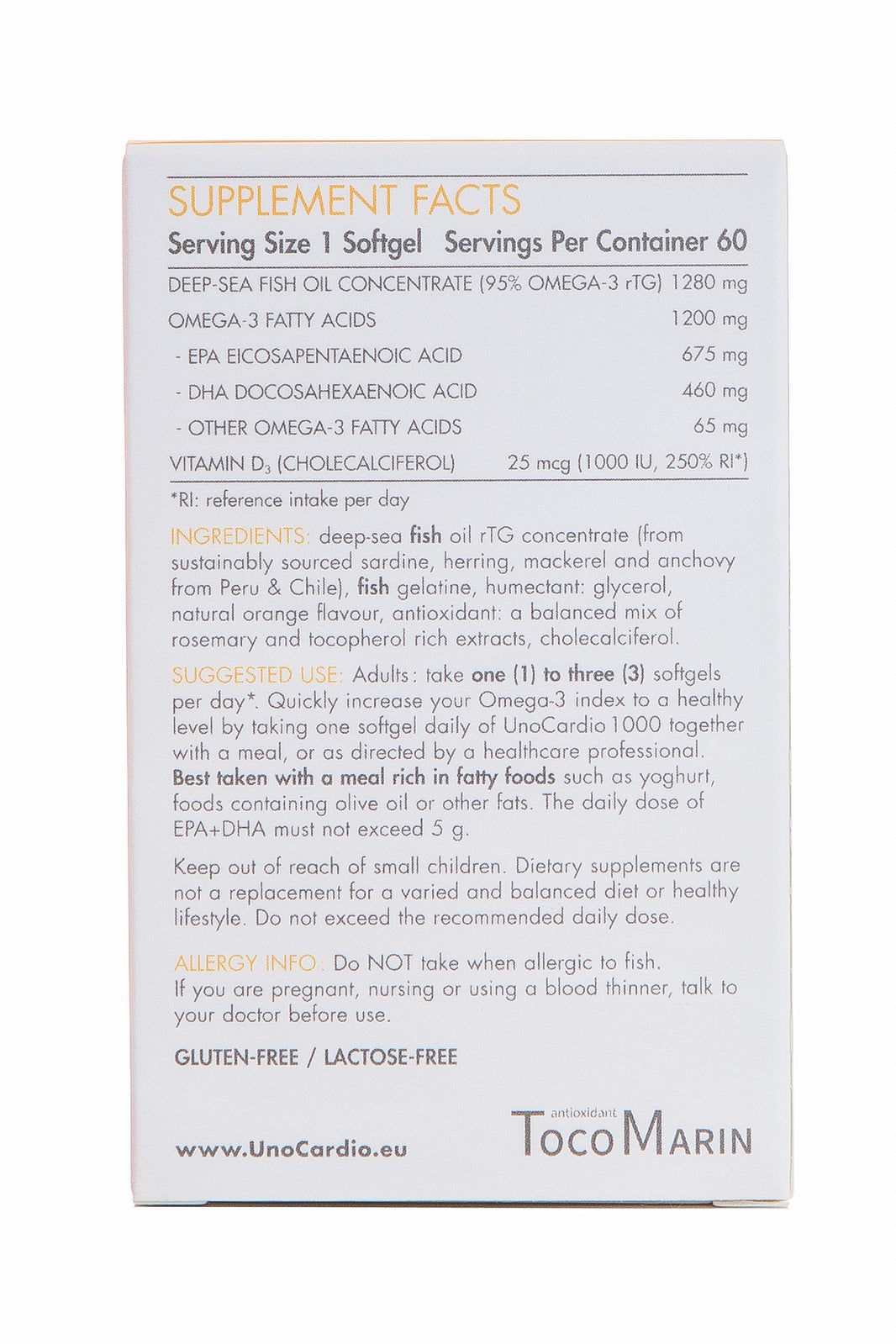
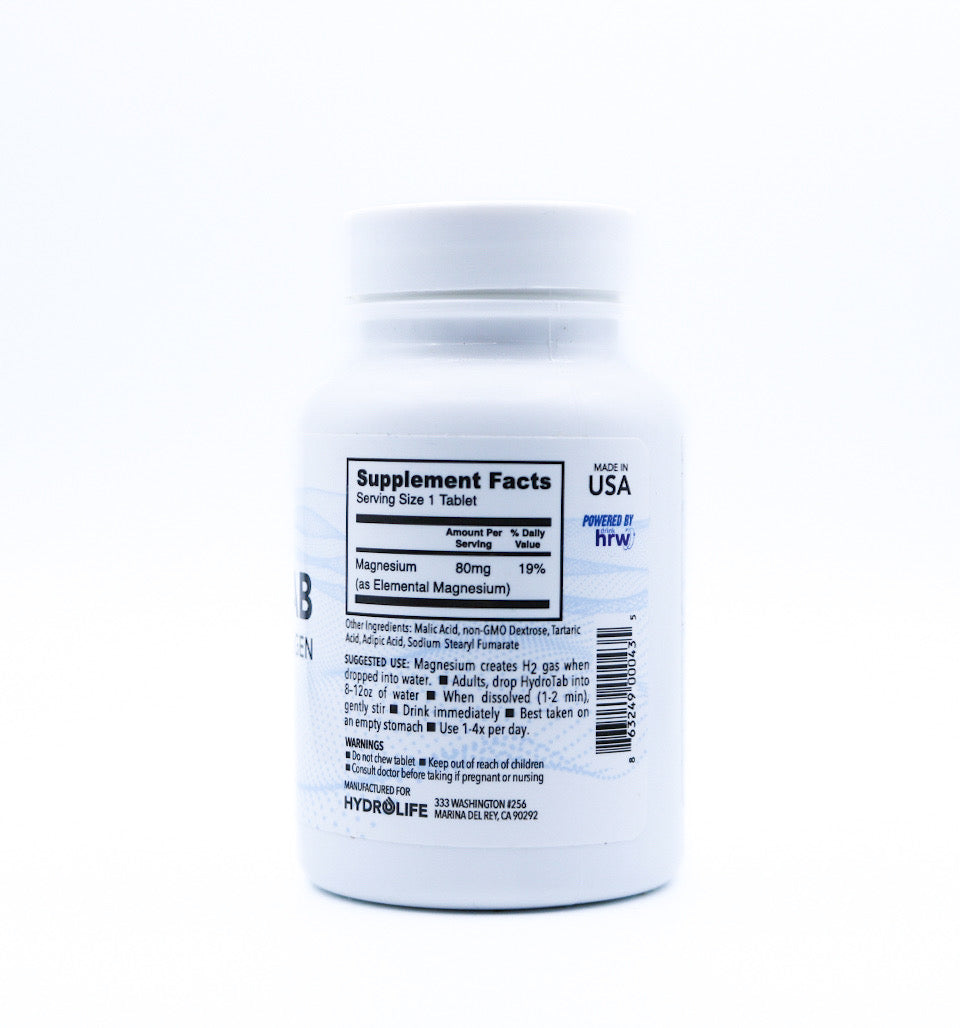
Take a look at our high quality blood sugar balance supplement collection here.
References
- Watson, S. (2019, March 26). How insulin works. WebMD. https://www.webmd.com/diabetes/insulin-explained
- Villines, Z. (2023, February 15). Insulin and glucagon: How They Regulate Blood Sugar Levels. Www.medicalnewstoday.com; Medical News Today. https://www.medicalnewstoday.com/articles/316427
- What is Glycogen and Why Does This Matter for Your Health? (2023, December 20). Healthline. https://www.healthline.com/health/nutrition/what-is-glycogen
- Echeverri, A. F., & Tobón, G. J. (2013). Autoimmune diabetes mellitus (Type 1A). In www.ncbi.nlm.nih.gov. El Rosario University Press. https://www.ncbi.nlm.nih.gov/books/NBK459476/
- Diabetes UK. (2023). Diabetes risk factors. Diabetes Uk. https://www.diabetes.org.uk/diabetes-the-basics/types-of-diabetes/type-2/diabetes-risk-factors
- How Sugar Converts to Fat. (2018, August 22). University of Utah Health | University of Utah Health. https://healthcare.utah.edu/the-scope/health-library/all/2018/08/how-sugar-converts-fat
- Riley, L. (2022). Mean Fasting Blood Glucose. World Health Organization. https://www.who.int/data/gho/indicator-metadata-registry/imr-details/2380
- Team, T. L. (2022, July 9). What are normal levels of insulin and why don’t we test it more? Levels. https://www.levels.com/blog/what-are-normal-insulin-levels-and-why-dont-we-test-it-more
- Cloyd, J. (2024, January 2). A functional medicine approach to prediabetes. Rupa Health. https://www.rupahealth.com/post/a-functional-medicine-approach-to-prediabetes
- Straus, D. S. (1981). Effects of insulin on cellular growth and proliferation. Life Sciences, 29(21), 2131–2139. https://doi.org/10.1016/0024-3205(81)90482-3
- Muniyappa, R., & Sowers, J. R. (2013). Role of insulin resistance in endothelial dysfunction. Reviews in Endocrine and Metabolic Disorders, 14(1), 5–12. https://doi.org/10.1007/s11154-012-9229-1
- Imai, S., Kajiyama, S., Kitta, K., Miyawaki, T., Matsumoto, S., Ozasa, N., Kajiyama, S., Hashimoto, Y., & Fukui, M. (2023). Eating Vegetables First Regardless of Eating Speed Has a Significant Reducing Effect on Postprandial Blood Glucose and Insulin in Young Healthy Women: Randomized Controlled Cross-Over Study. Nutrients, 15(5), 1174. https://doi.org/10.3390/nu15051174
- Mitrou, P., Petsiou, E., Papakonstantinou, E., Maratou, E., Lambadiari, V., Dimitriadis, P., Spanoudi, F., Raptis, S. A., & Dimitriadis, G. (2015). Vinegar Consumption Increases Insulin-Stimulated Glucose Uptake by the Forearm Muscle in Humans with Type 2 Diabetes. Journal of Diabetes Research, 2015, 1–7. https://doi.org/10.1155/2015/175204
- 9 foods to help lower blood sugar at home. (n.d.). Www.medicalnewstoday.com. https://www.medicalnewstoday.com/articles/322861
- Solomon, T. P. J., Tarry, E., Hudson, C. O., Fitt, A. I., & Laye, M. J. (2019). Immediate post-breakfast physical activity improves interstitial postprandial glycemia: a comparison of different activity-meal timings. Pflügers Archiv - European Journal of Physiology, 472(2), 271–280. https://doi.org/10.1007/s00424-019-02300-4






















Leave a comment