The human gut is a complex ecosystem that plays a crucial role in maintaining overall health. Beyond its primary function of digesting food and absorbing nutrients, the gut is intimately connected to the immune system. This connection, known as the gut-immune axis, highlights the importance of a healthy gut microbiome in supporting immune function.
The microbiome, consisting of trillions of microorganisms, including bacteria, fungi, and viruses, resides within the gut and significantly influences various aspects of health. A balanced and diverse microbiome is essential for optimal immune responses, as it helps to train and regulate the immune system. Conversely, an imbalanced or dysbiotic gut microbiome can contribute to immune dysfunction and the development of various health conditions. Understanding the gut-immune connection and the importance of a healthy microbiome is crucial for maintaining robust immune function and overall well-being.
Understanding the Gut Microbiome
The gut microbiome is a complex community of microorganisms that inhabit the gastrointestinal tract. It consists of a wide variety of bacteria, fungi, viruses, and other microbes, with bacteria being the most abundant. The composition of the gut microbiome is unique to each individual and is influenced by various factors, including genetics, age, diet, medication use, stress levels, and environmental exposures. A healthy gut microbiome is characterised by a diverse array of beneficial microbes that work together to maintain gut health and support immune function.
The beneficial bacteria in the gut play several key roles, such as breaking down complex carbohydrates, producing short-chain fatty acids, synthesising vitamins, and regulating the immune system. Some of the most well-known beneficial bacteria include Bifidobacteria and Lactobacilli, which are often found in probiotic supplements and fermented foods.
However, the gut microbiome can be easily disrupted by factors such as a diet high in processed foods, excessive antibiotic use, chronic stress, and environmental toxins. When the balance of the microbiome is disturbed, a state known as dysbiosis can occur, leading to an overgrowth of harmful bacteria and a reduction in microbial diversity. Dysbiosis has been linked to various health issues, including digestive problems, weakened immune function, and an increased risk of chronic diseases.
Maintaining a healthy gut microbiome is essential for overall health and can be achieved through a combination of dietary and lifestyle modifications. Consuming a diet rich in fibre, fermented foods, and prebiotics can help to support the growth of beneficial bacteria, while limiting processed foods, sugar, and excessive antibiotic use can help to prevent dysbiosis. Additionally, managing stress, engaging in regular exercise, and getting adequate sleep can all contribute to a healthy gut microbiome.
The Gut-Immune Connection

The gut and the immune system are intricately connected, with the gut playing a crucial role in the development and regulation of immune responses. The gut-associated lymphoid tissue (GALT) is the largest component of the body's immune system, accounting for approximately 70% of the entire immune system. The GALT is responsible for protecting the body against pathogens and other harmful substances that may enter through the gut.
The gut microbiome plays a significant role in the gut-immune connection. Beneficial bacteria in the gut interact with the immune cells in the GALT, helping to train and regulate immune responses. These bacteria can stimulate the production of various immune cells, such as T cells and B cells, which are essential for fighting off infections and maintaining immune balance.
Additionally, beneficial bacteria help to maintain the integrity of the gut barrier, which is a crucial line of defence against pathogens and toxins. The gut barrier consists of a single layer of epithelial cells that are tightly bound together by proteins called tight junctions. When the gut barrier is functioning properly, it prevents harmful substances from entering the bloodstream and triggering an immune response. However, when the gut barrier is compromised, a condition known as "leaky gut" can occur, allowing pathogens and toxins to enter the body and activate the immune system, leading to inflammation and other health issues.
Beneficial bacteria also help to protect the gut by competing with harmful pathogens for resources and attachment sites on the gut wall. By occupying these spaces, beneficial bacteria can prevent harmful pathogens from colonising the gut and causing infections.
Conversely, when the gut microbiome is imbalanced or dysbiotic, it can have negative consequences for immune health. Dysbiosis has been linked to various immune-related conditions, such as allergies, autoimmune disorders, and inflammatory bowel disease. In a state of dysbiosis, the gut barrier may become compromised, allowing harmful substances to enter the body and trigger an immune response. Additionally, a lack of beneficial bacteria can lead to an overgrowth of harmful pathogens, further exacerbating immune dysfunction.
Promoting a Healthy Gut Microbiome for Immune Support

Maintaining a healthy gut microbiome is essential for supporting immune function and overall health. There are several dietary and lifestyle strategies that can help to promote a balanced and diverse microbiome.
Dietary strategies
- Prebiotics: Prebiotics are non-digestible food components that serve as fuel for beneficial gut bacteria. They are found in various plant-based foods, such as garlic, onions, leeks, asparagus, and bananas. Consuming a diet rich in prebiotic foods can help to stimulate the growth and activity of beneficial bacteria in the gut.
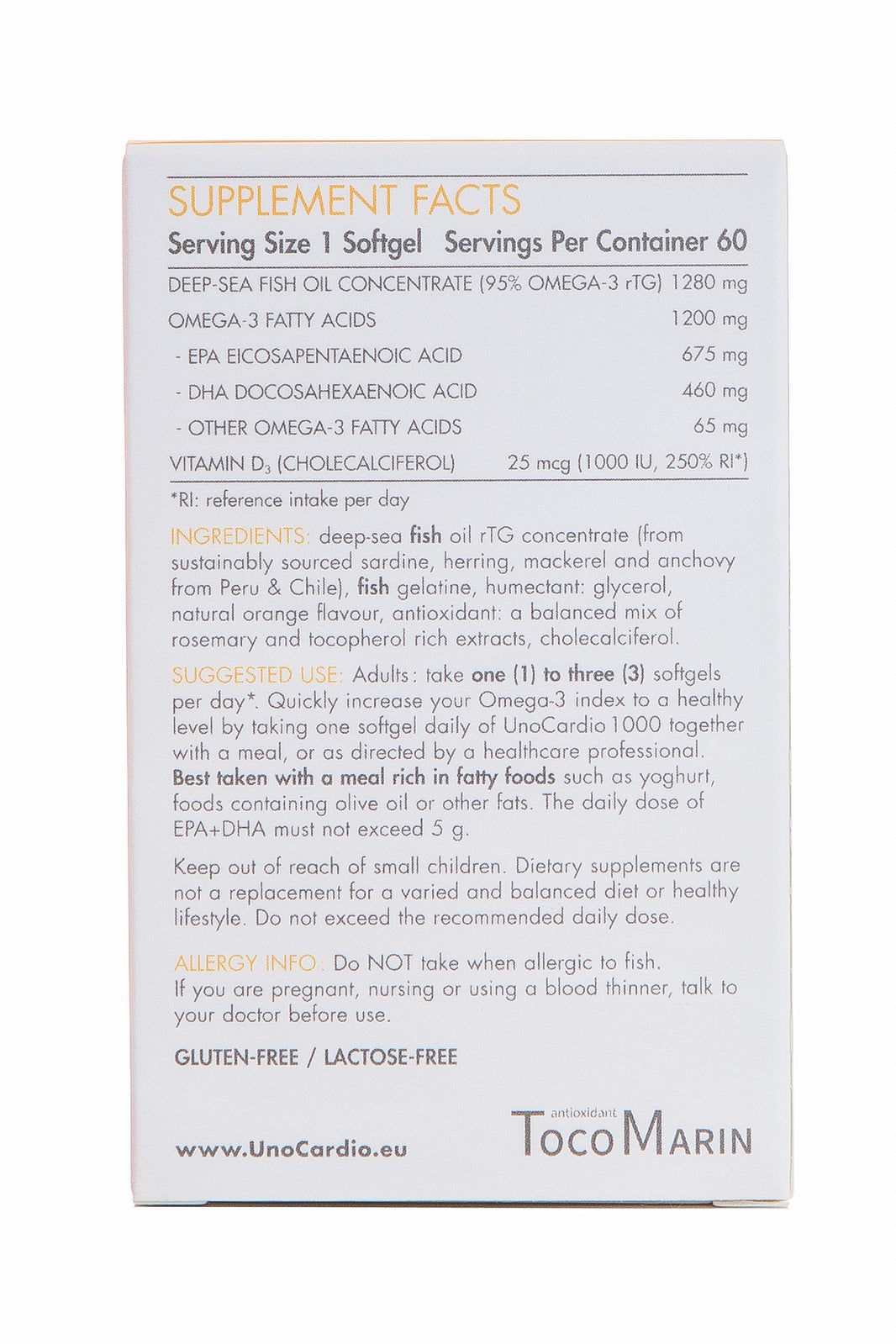
- Probiotics: Probiotics are live microorganisms that, when consumed in adequate amounts, can provide health benefits. They can be found in fermented foods, such as yoghurt, kefir, sauerkraut, and kimchi, as well as in supplement form. Probiotics can help to restore the balance of the gut microbiome and support immune function.
- Fermented foods: Fermented foods, such as yoghurt, kefir, sauerkraut, and kimchi, are rich in beneficial bacteria and can help to support a healthy gut microbiome. These foods have undergone a fermentation process, which allows beneficial bacteria to grow and multiply.
- Fibre-rich foods: Consuming a diet rich in fibre can help to support the growth and activity of beneficial gut bacteria. Fibre is found in various plant-based foods, such as fruits, vegetables, whole grains, and legumes. Fibre serves as a food source for beneficial bacteria, helping them to thrive and maintain a healthy gut microbiome.
Lifestyle modifications
- Managing stress: Chronic stress can have a negative impact on the gut microbiome, leading to dysbiosis and immune dysfunction. Engaging in stress-reducing activities, such as meditation, deep breathing, or yoga, can help to support a healthy gut microbiome and immune function.
- Regular exercise: Regular physical activity has been shown to have a positive impact on the gut microbiome. Exercise can help to increase the diversity of the microbiome and support the growth of beneficial bacteria. Aim for at least 150 minutes of moderate-intensity exercise per week.
- Adequate sleep: Getting enough quality sleep is essential for maintaining a healthy gut microbiome and immune function. Poor sleep has been linked to dysbiosis and immune dysfunction. Aim for 7-9 hours of sleep per night and practise good sleep hygiene, such as maintaining a consistent sleep schedule and creating a relaxing bedtime routine.
Cautious use of antibiotics and other medications
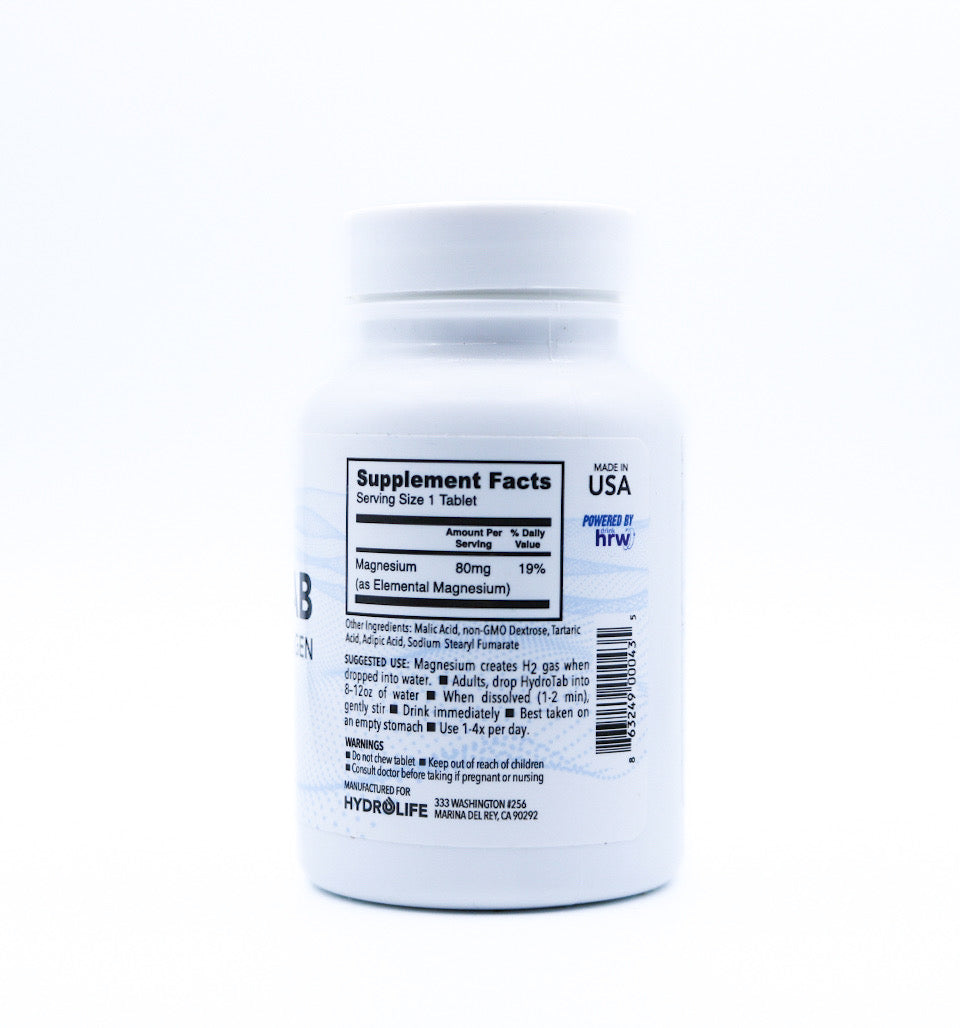
Antibiotics can be life-saving medications, but their overuse or misuse can have negative consequences for the gut microbiome. Antibiotics can disrupt the balance of the microbiome, leading to a reduction in beneficial bacteria and an overgrowth of harmful pathogens. When antibiotics are necessary, it is important to take them as prescribed and to consider using probiotic supplements to help restore the balance of the microbiome afterwards. Other medications, such as proton pump inhibitors and non-steroidal anti-inflammatory drugs, can also have negative impacts on the gut microbiome and should be used cautiously and under the guidance of a healthcare provider.
The Microbiome's Influence on Specific Immune Conditions

The gut microbiome has been implicated in various immune-related conditions, highlighting the importance of maintaining a healthy microbiome for optimal immune function.
- Allergies and asthma: Studies have shown that children who grow up in environments with a diverse array of microbes, such as farms or households with pets, are less likely to develop allergies and asthma. This is thought to be due to the early exposure to a wide range of microbes, which helps to train and regulate the immune system. Conversely, a lack of microbial diversity in the gut has been linked to an increased risk of allergies and asthma.
- Autoimmune disorders: The gut microbiome has been implicated in the development of various autoimmune disorders, such as rheumatoid arthritis, lupus, and multiple sclerosis. In these conditions, the immune system mistakenly attacks the body's own tissues, leading to inflammation and tissue damage. Dysbiosis of the gut microbiome has been observed in individuals with autoimmune disorders, suggesting that an imbalance of gut bacteria may contribute to the development and progression of these conditions.
- Inflammatory bowel disease: Inflammatory bowel disease (IBD), which includes Crohn's disease and ulcerative colitis, is characterised by chronic inflammation of the gastrointestinal tract. The gut microbiome has been implicated in the development and progression of IBD, with studies showing that individuals with IBD have a different gut microbiome composition compared to healthy individuals. Dysbiosis of the gut microbiome may contribute to the chronic inflammation seen in IBD.
- Respiratory infections: The gut microbiome has been shown to influence the risk and severity of respiratory infections, such as the common cold and influenza. A healthy gut microbiome can help to support immune function and reduce the risk of respiratory infections. Conversely, dysbiosis of the gut microbiome has been linked to an increased risk and severity of respiratory infections.
These examples highlight the important role that the gut microbiome plays in immune health and the development of various immune-related conditions. Maintaining a healthy gut microbiome through dietary and lifestyle modifications may help to support optimal immune function and reduce the risk of immune-related conditions.
Emerging Research and Future Directions

The field of gut microbiome research is rapidly evolving, with new insights and potential therapeutic strategies emerging regularly.
- Microbiome-based therapies: As our understanding of the gut microbiome's role in health and disease continues to grow, researchers are exploring the potential of microbiome-based therapies for various immune-related conditions. These therapies may involve the use of probiotics, prebiotics, or even faecal microbiota transplantation to modulate the gut microbiome and support immune function.
- Personalised nutrition based on microbiome profiles: Research has shown that the gut microbiome can influence an individual's response to different foods and dietary patterns. In the future, it may be possible to use an individual's microbiome profile to develop personalised nutrition plans that support optimal gut health and immune function.
- The potential of faecal microbiota transplantation: Faecal microbiota transplantation (FMT) involves the transfer of faecal matter from a healthy donor to an individual with a dysbiotic gut microbiome. FMT has shown promise in the treatment of recurrent Clostridium difficile infections and is being explored as a potential therapy for other immune-related conditions, such as inflammatory bowel disease and autoimmune disorders.
- The role of the microbiome in vaccine efficacy: Recent research has suggested that the gut microbiome may influence an individual's response to vaccines. Studies have shown that individuals with a healthy gut microbiome may have a better response to certain vaccines, such as the influenza vaccine, compared to those with a dysbiotic microbiome. Understanding the role of the microbiome in vaccine efficacy may help to develop strategies to optimise vaccine responses and protect against infectious diseases.
As research in this field continues to advance, it is likely that new insights and therapeutic strategies will emerge, highlighting the important role that the gut microbiome plays in immune health and overall well-being.
Conclusion: How a Healthy Microbiome Bolsters Your Immune System

The gut-immune connection is a complex and fascinating relationship that highlights the important role that the gut microbiome plays in overall health and well-being. The gut microbiome, consisting of trillions of microorganisms, interacts with the immune system in various ways, helping to train and regulate immune responses, maintain gut barrier integrity, and protect against harmful pathogens.
A healthy and diverse gut microbiome is essential for optimal immune function, as it helps to stimulate the production of immune cells, maintain the integrity of the gut barrier, and compete with harmful pathogens for resources and attachment sites on the gut wall. Conversely, an imbalanced or dysbiotic gut microbiome can contribute to immune dysfunction and the development of various immune-related conditions, such as allergies, autoimmune disorders, and inflammatory bowel disease.
Maintaining a healthy gut microbiome is crucial for supporting immune health and can be achieved through a combination of dietary and lifestyle modifications. Consuming a diet rich in prebiotics, probiotics, fermented foods, and fibre can help to support the growth and activity of beneficial gut bacteria. Additionally, managing stress, engaging in regular exercise, getting adequate sleep, and using antibiotics and other medications cautiously can all contribute to a healthy gut microbiome.
As research in this field continues to advance, it is becoming increasingly clear that the gut microbiome plays a critical role in immune health and overall well-being. By understanding the gut-immune connection and taking steps to support a healthy gut microbiome, individuals can help to optimise their immune function and reduce the risk of various health conditions. As new insights and therapeutic strategies emerge, the potential for microbiome-based interventions to support immune health and prevent disease is an exciting and promising area of research.
Discover the power of your gut: Embrace a healthier lifestyle today and unlock the key to enhancing your immune system with our tailored gut health solutions.
Further Reading
For further reading and exploration of the intricate connection between the gut microbiome and the immune system, the following resources provide in-depth insights and scientific research:
- The Role of Gut Microbiota in Immune Homeostasis and Autoimmunity: This article on NCBI delves into how gut microbes interact with the host immune system, influencing the development of autoimmune diseases. Read more about gut microbiota and immunity.
- Nutrition and Immunity - Harvard T.H. Chan School of Public Health: Harvard's resource explains how the immune system is influenced by various factors, including diet, and discusses the roles specific foods and nutrients play in maintaining immune health. Explore the relationship between nutrition and immunity.
- The Interplay between the Gut Microbiome and the Immune System: An article from NCBI that reviews the mechanisms involved in maintaining the balance between the microbiota, gut health, and the local immune response. Learn about the interplay between gut microbiome and immune system.
- The Compelling Link between Physical Activity and the Body's Defense System: This study from ScienceDirect discusses how physical activity influences the gut microbiota, which in turn affects human health and the immune system. Read about the connection between physical activity and immune health.
- The Role of Short-Chain Fatty Acids From Gut Microbiota in Gut-Brain Communication: Frontiers in Endocrinology explores how interactions between the microbiota, immune, and nervous systems affect health and disease. Understand the role of short-chain fatty acids.
Water for Health Ltd began trading in 2007 with the goal of positively affecting the lives of many. We still retain that mission because we believe that proper hydration and nutrition can make a massive difference to people’s health and quality of life. Click here to find out more.























Leave a comment