Cholesterol. It's a word that sends shivers down the spines of many, conjuring images of clogged arteries and ticking time bombs. Yet, the story of cholesterol, like most things in functional medicine, is far more nuanced than just "good" versus "bad." While high cholesterol levels can indeed increase heart disease risk, focusing solely on a single number from a standard lipid panel paints an incomplete, and potentially misleading, picture of your cardiovascular health.
As a functional nutritional therapist, I see it all too often – individuals fixated on lowering their total cholesterol at all costs, often overlooking crucial details that paint a more holistic picture of their body's inner workings. It's time to move beyond the limitations of standard cholesterol testing and embrace a more comprehensive approach to assessing your heart health.
Why Standard Cholesterol Testing Falls Short:
Traditional lipid panels offer a basic snapshot of your cholesterol levels, typically measuring total cholesterol, LDL ("bad" cholesterol), HDL ("good" cholesterol), and triglycerides. While these numbers hold some value, they often fail to capture the complexities of cholesterol metabolism and its impact on heart health. Here's why:
1. The "Good" and the "Bad" Aren't So Simple:
- LDL isn't all created equal: Lumping all LDL cholesterol into one category ignores the crucial distinction between large, fluffy LDL particles and small, dense LDL particles. The latter are more prone to sticking to artery walls and contributing to plaque buildup, posing a more significant threat to heart health. Standard panels don't differentiate between these types, potentially missing individuals with high small-particle LDL despite "normal" overall LDL levels.
- HDL complexity: Yes, HDL, often referred to as "good" cholesterol, helps remove LDL from the bloodstream. But not all HDL functions equally. Studies suggest that larger HDL particles are more effective at carrying LDL away from arteries, while smaller HDL particles may be less efficient [1]. Standard panels typically don't distinguish between HDL particle sizes, limiting the information they provide.
2. Ignoring Key Players:
Standard panels miss out on other crucial actors in the heart health drama:
- ApoB: This protein particle binds to fats like LDL and triglycerides, playing a pivotal role in cholesterol transport and potentially contributing to heart disease risk. Measuring ApoB can provide a more comprehensive view of cardiovascular risk than just looking at individual lipid levels [2].
- Triglycerides: While often overshadowed by cholesterol, high triglycerides, particularly in combination with low HDL, can independently increase heart disease risk. Standard panels include triglycerides, but a deeper dive into their relationship with other lipids and metabolic markers can provide further insights.
3. One Size Doesn't Fit All:
Target cholesterol levels set by traditional guidelines may not be optimal for everyone. Individual factors like age, genetics, family history, and overall health status need to be considered. Focusing solely on a single number can lead to unnecessary interventions or missed opportunities for targeted approaches.
Embracing a Functional Approach to Heart Health Assessment:

So, what's the solution? Ditch the fearmongering and move towards a functional approach that empowers you to gain a deeper understanding of your individual heart health landscape. This involves:
1. Expanding Your Testing Toolbox:
Several advanced tests can provide a more comprehensive picture of your cardiovascular risk:
- NMR LipoProfile: This test analyses the size and number of LDL and HDL particles, offering valuable insights into the risk associated with your specific cholesterol profile [3].
- ApoB testing: Measuring ApoB levels can provide a more accurate assessment of total atherogenic lipoprotein particles, potentially offering a clearer picture of cardiovascular risk [4].
- Triglyceride-rich lipoprotein (TRL) testing: This test measures specific types of lipoproteins rich in triglycerides, offering further insights into metabolic health and heart disease risk [5].
2. Don't Demonise Cholesterol:
Remember, cholesterol is essential for various bodily functions, including hormone production and cell membrane integrity. Demonising it altogether can be counterproductive. The focus should be on optimising its metabolism and ensuring the right balance between different types and particle sizes.
3. Consider Functional Medicine Insights:
Functional medicine practitioners delve deeper, exploring potential underlying factors contributing to imbalanced cholesterol levels, such as:
- Insulin resistance: This condition, linked to high blood sugar and refined carbohydrate intake, can contribute to small, dense LDL particles and increased triglyceride levels [6].
- Inflammation: Chronic inflammation, often driven by gut imbalances, food sensitivities, or stress, can contribute to a more atherogenic lipid profile [7].
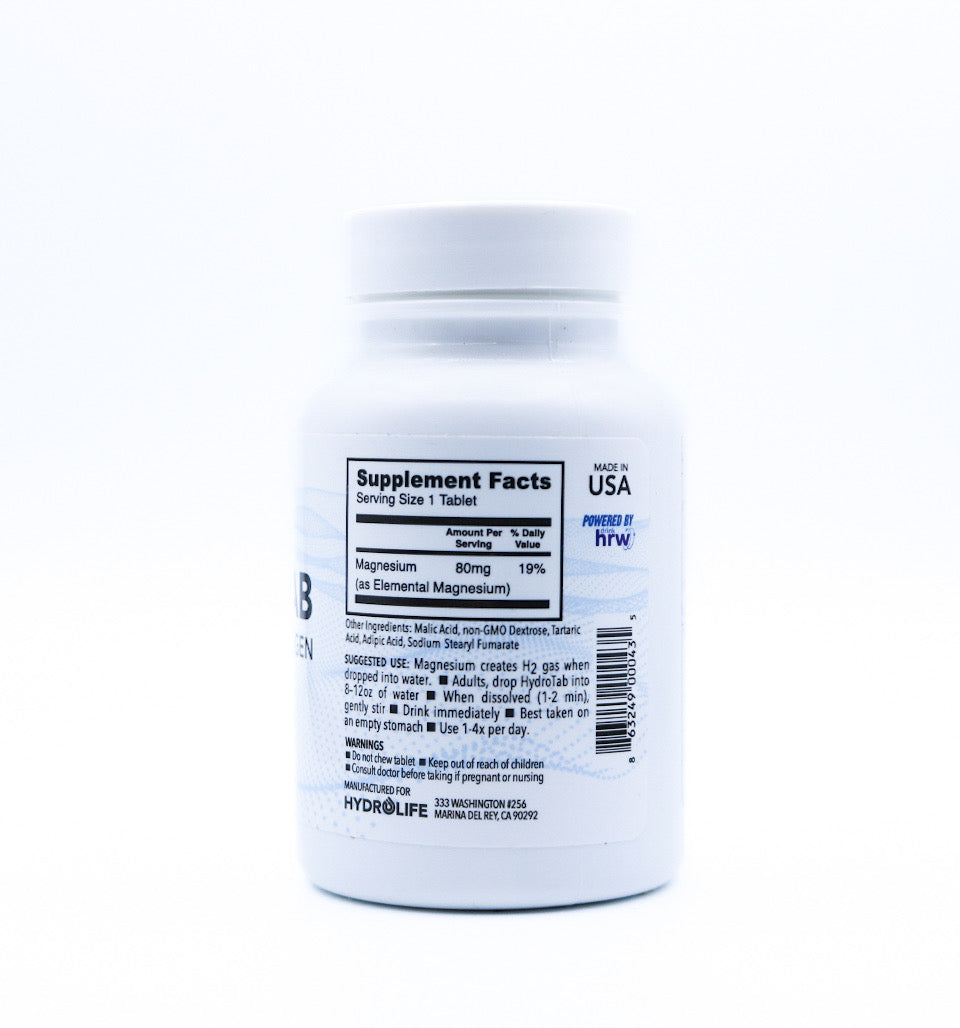
- Nutrient deficiencies: Deficiencies in essential nutrients like magnesium, B vitamins, and antioxidants can impact cholesterol metabolism and heart health [8, 9].
- Individualised Action Plans: Based on your comprehensive assessment, your functional medicine practitioner can create a personalised roadmap for optimising your heart health. This may include:
- Dietary interventions: Focusing on whole, unprocessed foods, healthy fats, fibre, and moderate protein intake while limiting refined carbohydrates, sugary drinks, and unhealthy fats can significantly impact your lipid profile and overall cardiovascular health [10].
- Lifestyle modifications: Regular exercise, stress management techniques, and adequate sleep are crucial for optimal heart health and can positively impact cholesterol metabolism [11, 12].
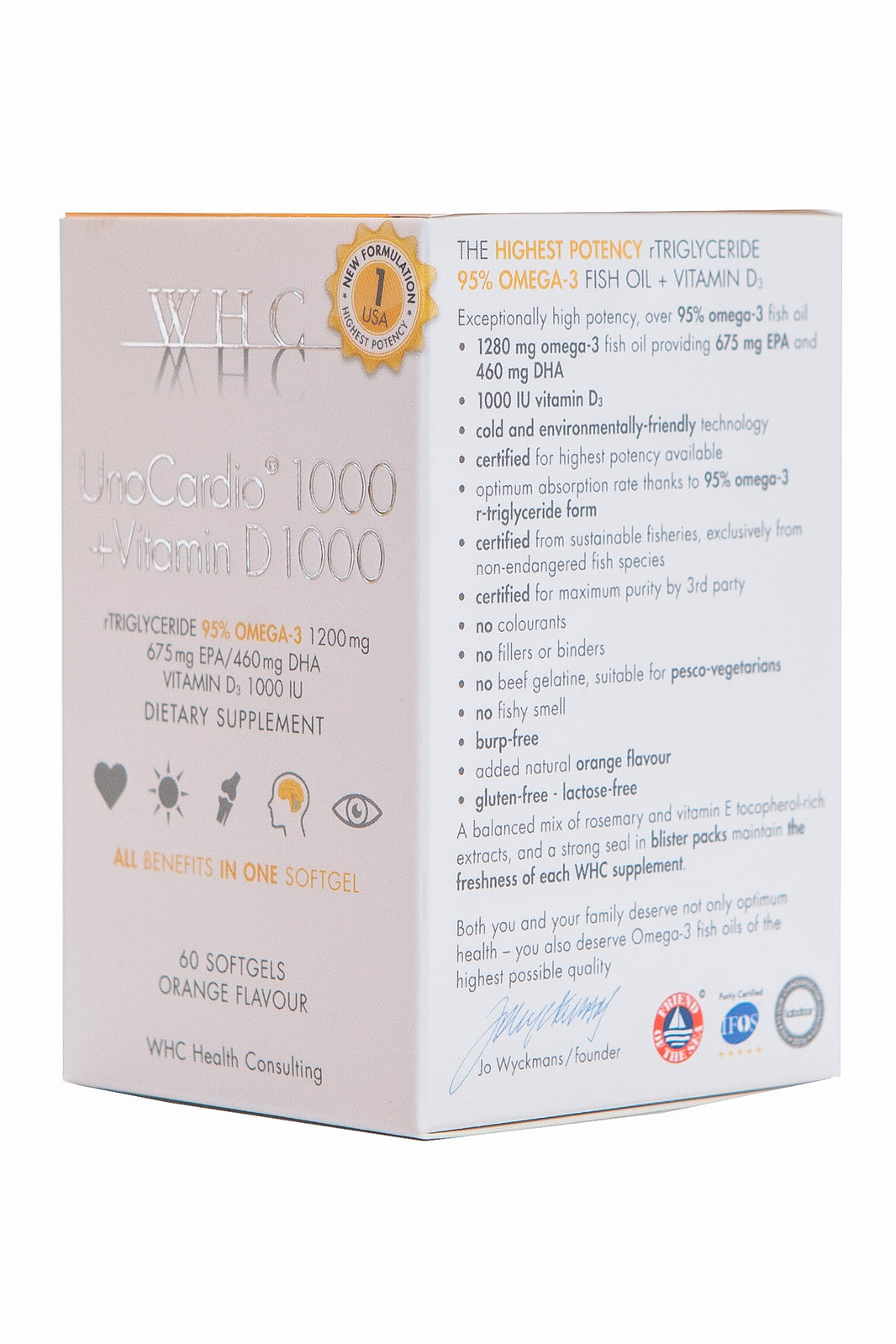
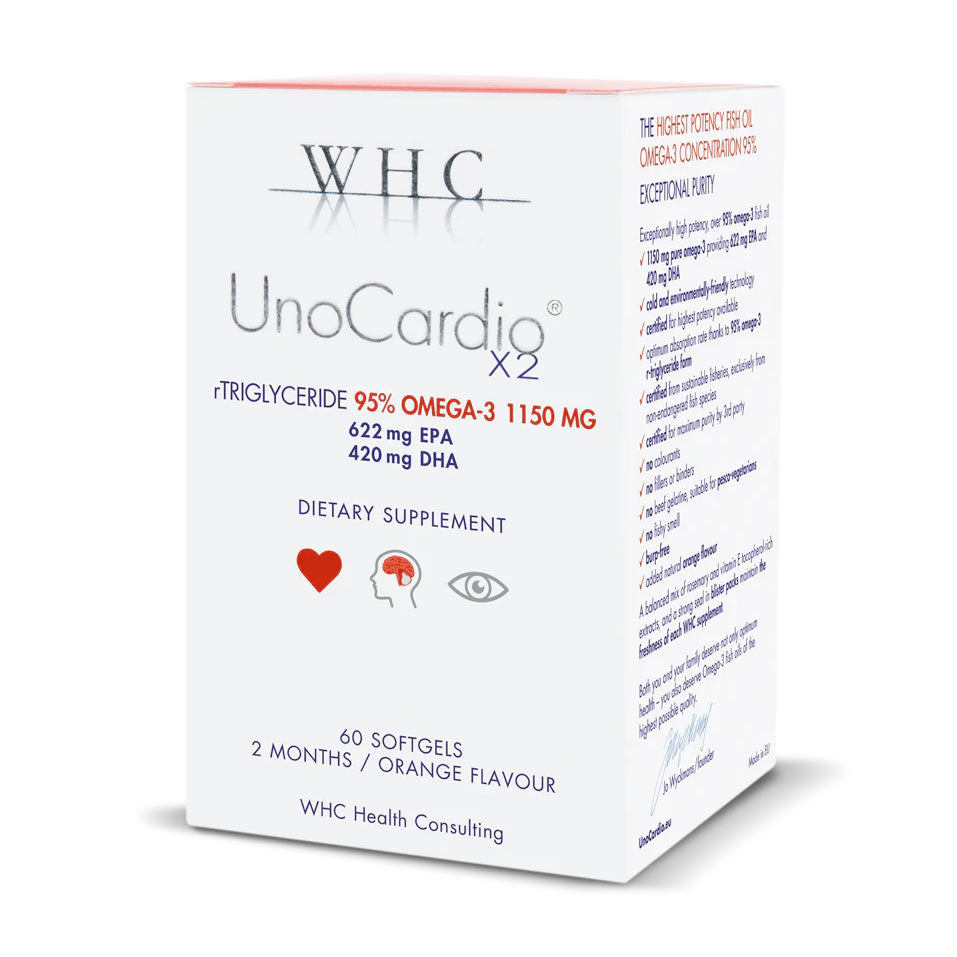
- Targeted supplementation: Addressing nutrient deficiencies and supporting healthy inflammation levels with targeted supplements like magnesium, fish oil, and curcumin can offer additional benefits [13, 14].
- Functional medicine modalities: Depending on your individual needs, your practitioner may recommend modalities like gut health protocols, herbal remedies, or acupuncture to address underlying imbalances and support heart health holistically.
Remember, you are not just a (cholesterol) number.
Taking a functional approach to heart health empowers you to move beyond the limitations of standard testing and understand your unique risk factors. By delving deeper, creating an individualised plan, and prioritising a holistic approach, you can optimise your cholesterol profile, address potential underlying imbalances, and truly take charge of your heart health journey.
But remember, this is just the first step. Optimising your heart health is an ongoing process that requires commitment, consistency, and collaboration with a healthcare professional who understands your unique needs and goals. Don't hesitate to seek guidance from a qualified functional medicine practitioner or integrative healthcare provider who can support you on this journey. Together, you can unlock the full potential of your heart health and live a long, vibrant life.
Empower yourself with knowledge, embrace a personalised approach, and take control of your heart's well-being. Your heart will thank you for it.
Written by Amy Morris, BSc (Hons) Nutritional Therapy. Amy has been a nutritional therapist for 12 years, specialising in recent years as a functional medicine nutritional therapist. Women’s health, and pre-diabetes and type 2 diabetes prevention are Amy’s specialist areas. Diagnosed with a chronic condition called endometriosis at age 20, this is what motivated Amy to study nutrition. Amy has been in remission for 6 years now, attributing powerful nutrition, lifestyle and bio-identical hormone strategies she now shares with her clients.
Water for Health Ltd began trading in 2007 with the goal of positively affecting the lives of many. We still retain that mission because we believe that proper hydration and nutrition can make a massive difference to people’s health and quality of life. Click here to find out more.
References:
[1] Barter PJ, Rye KA, Thompson PL. HDL cholesterol: a therapeutic target for preventing and treating coronary heart disease. Eur Heart J. 2004;25(23):2206-2215. doi:10.1016/s0195-668x(04)00402-5
[2] Nordestgaard BT, Chapman MJ, Descamps OS, et al. Apolipoprotein B: a comprehensive assessment of its role as a causal variable in atherogenesis. Eur Heart J. 2020;41(9):1105-1115. doi:10.1093/eurheartj/ehz351
[3] Nordestgaard BT, Benn M, Tybjaerg-Hansen A, et al. Lipoprotein(a) as a causal risk factor for ischemic heart disease: results from a large Danish cohort study. Eur Heart J. 2017;38(22):1705-1712. doi:10.1093/eurheartj/ehx199
[4] Nordestgaard BT, Chapman MJ, Descamps OS, et al. Apolipoprotein B: a comprehensive assessment of its role as a causal variable in atherogenesis. Eur Heart J. 2020;41(9):1105-1115. doi:10.1093/eurheartj/ehz351
[5] Hegele RA, Packard CJ. Triglyceride-rich lipoproteins: new insights into their heterogeneity and role in metabolic syndrome. Clin Chem. 2005;51(6):1191-1199. doi:10.1373/clinchem.2005.057222
[6] Grundy SM, Cleeman CL, Merz CN, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III Guidelines. Circulation. 2004;109(21):2844-2848. doi:10.1161/01.cir.0000133824.47138.b7
[7] Libby P, Ridker PM, Hansson GK. Inflammation in atherosclerosis: from pathophysiology to paradigm shift. Nat Rev Cardiol. 2011;8(12):691-702. doi:10.1038/nrcardio.2011.96
[8] Rayson MP, King DE, Proudfoot JL, et al. Magnesium supplementation for reducing blood pressure: a systematic review and meta-analysis. J Am Coll Cardiol. 2016;67(6):604-618. doi:10.1016/j.jacc.2015.11.029
[9] Wang H, Sun X, Li T, et al. Effect of B vitamin supplementation on serum homocysteine and vascular risk factors in hypertensive patients: a meta-analysis. Am J Clin Nutr. 2014;99(2):246-254. doi:10.3945/ajcn.11304755
[10] Dietary Guidelines for Americans, 2020-2025. U.S. Department of Agriculture and U.S. Department of Health and Human Services. https://www.myplate.gov/
[11] Warburton DE, Nicol CW, Bredin SS. Health benefits of physical activity: the evidence. Can J Appl Physiol. 2006;31(4):449-485. doi:10.1139/h06-041
[12] McEwen BS. The effect of stress on human health and hormone function. J Neuroendocrinol. 2006;18(3):138-148. doi:10.1111/j.1365-2553.2005.01470.x
[13] Cicero AFG, Fogacci F, Colletti A, et al. Long-chain omega-3 fatty acids and coronary heart disease: a meta-analysis of randomized controlled trials. Am J Clin Nutr. 2011;93(4):770-782. doi:10.3945/ajcn.110.007964
[14] Aggarwal BB, Harikumar KB. Potential therapeutic effects of curcumin, the anti-inflammatory agent, in neurodegenerative diseases: a review. J Am Assoc Physicians Ind. 2009;57(4):195-203.