When it comes to our mental health, the discussion often loops back to a handful of neurotransmitters. Serotonin, the 'happiness neurotransmitter', and its amine siblings, dopamine and norepinephrine, have long held the spotlight in the realm of depression. However, recent years have unveiled a far more complex narrative -- one that reevaluates depression not merely as a shortage of these mood-modulating chemicals, but as a symptom of a wider-reaching, invisible health culprit: chronic inflammation.
The Serotonin Paradox and the Role of Inflammation
For decades, medical lore has woven the tale that depression springs from a deficiency in serotonin and other neurotransmitters. After all, the 'Prozac revolution' of the 80s and 90s cemented this belief, linking depression to the need for a ‘chemical fix’. Yet, scepticism has grown. A pioneering meta-analysis, conducted by UCL researchers (1), found no substantial proof to verify the low-serotonin hypothesis. Instead, the data paints a more puzzling picture: depressed individuals who use antidepressants often exhibit even lower levels of serotonin, pointing to a 'chicken or the egg' conundrum that upends our traditional understanding of depression causality.

Conversely, a wealth of new research suggests that inflammation could be a critical piece of the puzzle (2). Inflammation, which usually springs into action as the body's defence mechanism against infections and injuries, is becoming a prime suspect in driving depressive symptoms. The immune system, when on high alert, can release a cascade of cytokines that signal the brain and prime it to enter a 'sickness state' marked by social withdrawal, reduced motivation, and anhedonia -- classic markers of depression.
This emerging paradigm, popularised by health leaders like Chris Kresser, unravels depression as not just a mental illness but possibly a 'disease of inflammation'. It's a notion supported by various studies, including trials where administering inflammatory cytokines to otherwise healthy individuals resulted in the onset of depressive symptomatology. The implications are profound, suggesting that the roots of depression could be as deeply entwined with our bodily health as with our mental well-being.
Depression as a Symptom, Not a Standalone Illness
It's essential to recognise that depression is often a symptom, rather than the disease itself. Much like a fever alerts us to an underlying infection, depression might be the body's signal of an internal imbalance. This shift in perspective opens up a trove of potential causes beyond neurotransmitter levels.
Digging Deeper into Underlying Causes
Many medical conditions can masquerade as depression, often leading to misdiagnosis and mistreatment. From insidious pathologies like an under active thyroid or low iron levels to more apparent culprits like chronic stress, the range of potential depression instigators is vast. Each requires a unique approach and highlights the need for comprehensive evaluations rather than quick-fix solutions or medication alone.
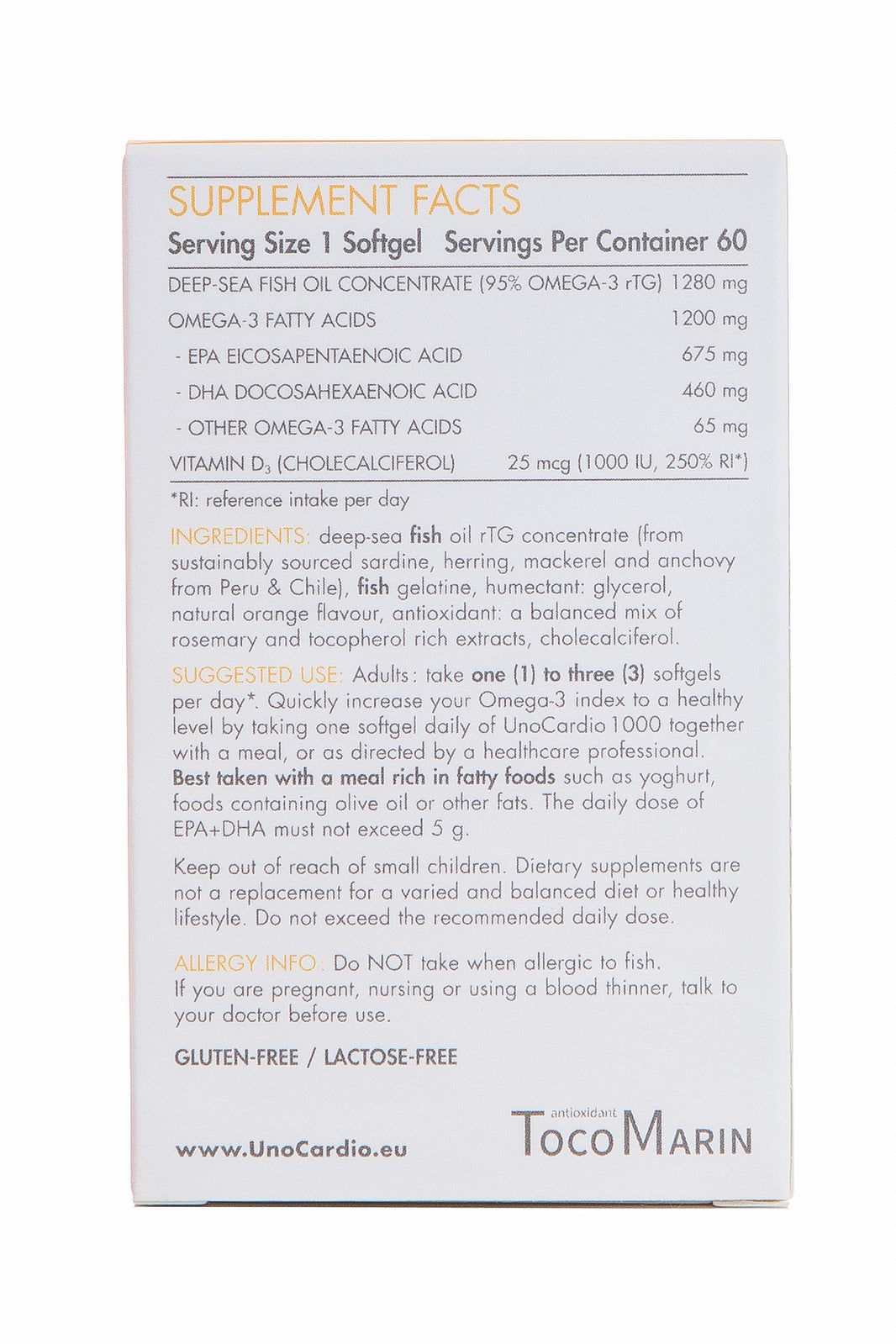
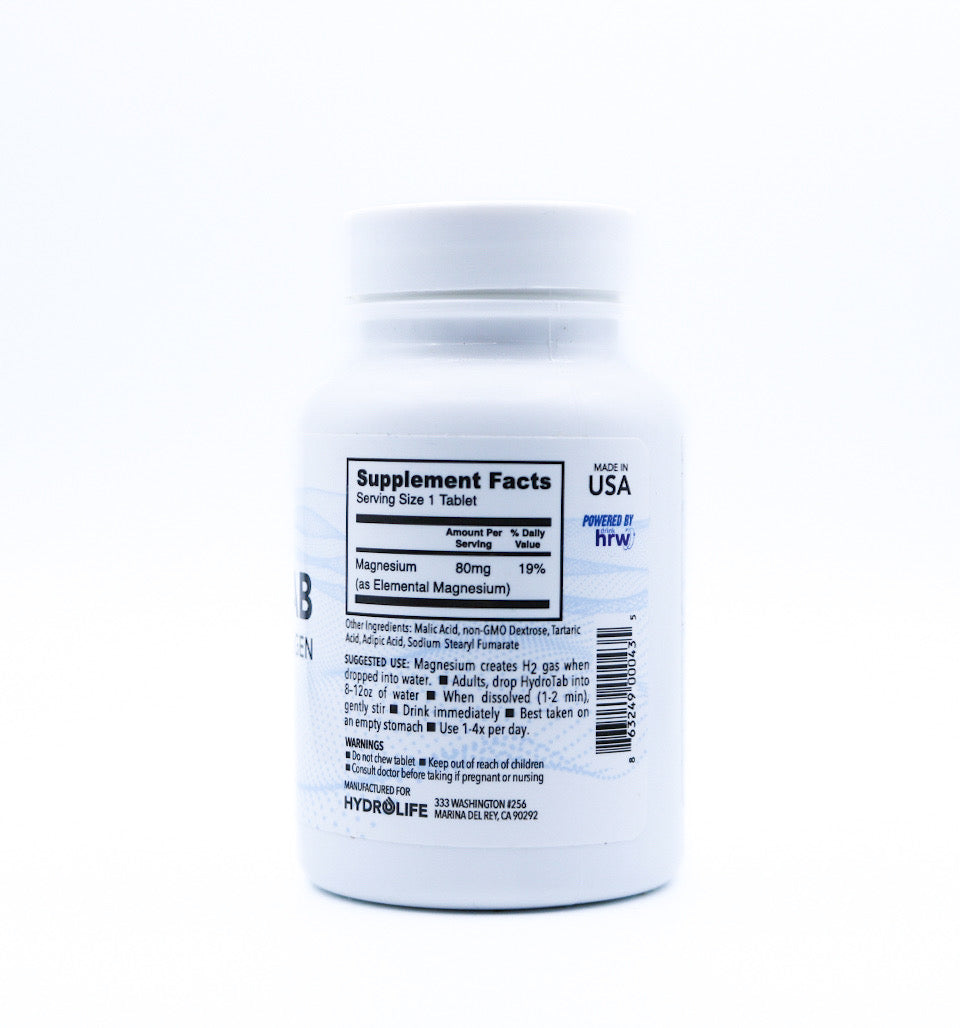
Chronic infections, for instance, draw on the immune system's resources for prolonged periods, often leading to fatigue and malaise that eerily mimic depressive symptoms. Meanwhile, nutrient deficiencies, such as a lack of vitamin D (3) or omega-3 fatty acids (4), have been linked to higher rates of depression and underscore the importance of a nutritionally rich diet.
Addressing the Causes, Not Just the Symptoms
Recognising depression as a symptom spurs a shift in the therapeutic approach, one that prioritises addressing the root causes. Top on the list of actionable strategies is lifestyle intervention. Diet, exercise, and sleep, often overlooked in the mental health discourse, wield significant influence over our inner inflammatory landscape.

Anti-inflammatory diets, rich in fruits, vegetables, omega-3 fatty acids, and probiotics, have been shown to reduce systemic inflammation and improve mood (5). Contrastingly, high-sugar diets and the traditional Western diet, laden with processed foods (6), can stoke the fires of inflammation and exacerbate depressive symptoms.
Physical activity, a renowned anti-inflammatory, has been lauded for its mood-enhancing properties. Its effects on brain-derived neurotrophic factor (BDNF) (7) akin to fertiliser for the brain, cultivating neuroplasticity and resilience. Sleep, a critical pillar of health, carves its niche in the depression-inflammation alliance with sleep deprivation potentiating cytokine release and inflammatory processes in the body (8).
Stress management and social connectedness round out the lifestyle considerations, with mindfulness practices (9) and supportive relationships (10) offering bulwarks against the wear and tear of chronic stress and the spike in inflammation it can elicit.
Unlocking the Healing Potential
Understanding depression through the lens of inflammation provides a richer comprehension and, more importantly, a broader palette of options for treatment and prevention. Personalising interventions to address the specific inflammatory signals at play could be the turning point for many struggling with depression.
Personalised Medicine for Depression
Identifying the inflammatory triggers in each individual demands a customised diagnostic approach. Functional medicine, with its focus on patient-centered care and the interplay between genetics and environment, offers a template for tailored assessments. Comprehensive lab work, including inflammation markers and nutritional status, can illuminate the path forward, guiding practitioners and patients toward the interventions that hold the most promise.
Integrative and Holistic Care
The shift towards an integrative model of care, merging the best of conventional and complementary practices, is vital. Combining talk therapy with dietary changes, acupuncture with pharmaceuticals, or yoga with medication can furnish a more comprehensive approach, leveraging the strengths of each modality while mitigating their limitations.
The Importance of Patient Empowerment
Empowering individuals with the knowledge and tools to manage their inflammatory status is equally crucial. Patient education on the role of diet, exercise, and stress reduction in modulating inflammation can equate to long-term self-management of depressive symptoms that go beyond the scope of a therapist's chair or a doctor's prescription pad.
The Path Forward For Depression As a Symptom
The burgeoning connection between inflammation and depression is rapidly reshaping our perspective on mental health. Shifting the focus from neurotransmitters to the body's internal inflammatory milieu opens up a new world of possibilities for healing and hope for the millions navigating the dense fog of depression.
It is a paradigm that calls for a medical community willing to pivot, research that dares to venture beyond the serotonin spotlight, and a society ready to shun one-size-fits-all solutions in favour of individualised, root cause-focused strategies. By weaving this multifaceted tapestry of lifestyle changes, nutritional support, integrative therapies, and patient empowerment, we inch closer to a future where depression is not just managed, but understood, and ultimately, prevented.
This is the frontier of mental health -- an uncharted territory brimming with opportunities to redefine our approach and, in the process, redefine our lives. The call to action echoes louder with each groundbreaking study and each anecdote of transformation: we must look beyond the surface, beyond the serotonin, to truly comprehend the enigma of depression.
In doing so, we arm ourselves with the knowledge to ebb the tide of chronic inflammation and, perhaps, liberate the many ensnared by the silent suffering of depression. The task is daunting, but the stakes could not be higher. It is a mission that transcends specialties, blurs the lines between mind and body, and unites us in a shared endeavour to unveil the multifaceted nature of depressive disorders. Through this lens, we not only glimpse new horizons in treatment but also kindle the fire of hope for a future where mental health is truly within reach for all.
Written by Amy Morris, BSc (Hons) Nutritional Therapy. Amy has been a nutritional therapist for 12 years, specialising in recent years as a functional medicine nutritional therapist. Women’s health, and pre-diabetes and type 2 diabetes prevention are Amy’s specialist areas. Diagnosed with a chronic condition called endometriosis at age 20, this is what motivated Amy to study nutrition. Amy has been in remission for 6 years now, attributing powerful nutrition, lifestyle and bio-identical hormone strategies she now shares with her clients. https://www.greathealthnaturally.co.uk/
Water for Health Ltd began trading in 2007 with the goal of positively affecting the lives of many. We still retain that mission because we believe that proper hydration and nutrition can make a massive difference to people’s health and quality of life. Click here to find out more.
References
References:
1) Moncrieff, J., Cooper, R. E., Stockmann, T., Amendola, S., Hengartner, M. P., & Horowitz, M. A. (2022, July). No evidence that depression is caused by low serotonin levels, finds comprehensive review. UCL News. https://www.ucl.ac.uk/news/2022/jul/no-evidence-depression-caused-low-serotonin-levels-finds-comprehensive-review
2) Berk, M., Williams, L.J., Jacka, F.N., et al. (2013). So depression is an inflammatory disease, but where does the inflammation come from? BMC Medicine, 11, 200. https://doi.org/10.1186/1741-7015-11-200
3) Akpınar, Ş., & Karadağ, M. G. (2022). Is Vitamin D Important in Anxiety or Depression? What Is the Truth?. Current nutrition reports, 11(4), 675–681. https://doi.org/10.1007/s13668-022-00441-0
4) Mehdi, S., Manohar, K., Shariff, A., Kinattingal, N., Wani, S. U. D., Alshehri, S., Imam, M. T., Shakeel, F., & Krishna, K. L. (2023). Omega-3 Fatty Acids Supplementation in the Treatment of Depression: An Observational Study. Journal of personalized medicine, 13(2), 224. https://doi.org/10.3390/jpm13020224
5) Kurowska, A., Ziemichód, W., Herbet, M., & Piątkowska-Chmiel, I. (2023). The Role of Diet as a Modulator of the Inflammatory Process in the Neurological Diseases. Nutrients, 15(6), 1436. https://doi.org/10.3390/nu15061436
6) Ma, X., Nan, F., Liang, H., Shu, P., Fan, X., Song, X., Hou, Y., & Zhang, D. (2022). Excessive intake of sugar: An accomplice of inflammation. Frontiers in immunology, 13, 988481. https://doi.org/10.3389/fimmu.2022.988481
7) Sleiman, S. F., Henry, J., Al-Haddad, R., El Hayek, L., Abou Haidar, E., Stringer, T., Ulja, D., Karuppagounder, S. S., Holson, E. B., Ratan, R. R., Ninan, I., & Chao, M. V. (2016). Exercise promotes the expression of brain derived neurotrophic factor (BDNF) through the action of the ketone body β-hydroxybutyrate. eLife, 5, e15092. https://doi.org/10.7554/eLife.15092
8) Lee, C. H., & Giuliani, F. (2019). The Role of Inflammation in Depression and Fatigue. Frontiers in immunology, 10, 1696. https://doi.org/10.3389/fimmu.2019.01696
9) Carmody, J., & Baer, R. A. (2008). Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. Journal of Behavioral Medicine, 31(1), 23-33. https://www.researchgate.net/publication/5946075_Relationships_between_mindfulness_practice_and_levels_of_mindfulness_medical_and_psychological_symptoms_and_well-being_in_a_mindfulness-based_stress_reduction_program
10) Fagundes, C. P., Bennett, J. M., Derry, H. M., & Kiecolt-Glaser, J. K. (2011). Relationships and Inflammation across the Lifespan: Social Developmental Pathways to Disease. Social and personality psychology compass, 5(11), 891–903. https://doi.org/10.1111/j.1751-9004.2011.00392.x


























Leave a comment