Research is continually evolving, and scientists are discovering an increasing amount about the complexity of our digestive system and how vital it is when it comes to our health.
Around 70% of your immune system stems from your GI tract, all the way from your mouth, through your throat, oesophagus, stomach, small intestine, large intestine, rectum and anus.
A healthy gut is integral to your overall health, and without it, you become more susceptible to a poorly functioning immune system, chronic disease of all kinds, mental health disorders, endocrine disorders and skin conditions.
Every one of us has an assortment of gut microbiota, or microorganisms, as unique as our fingerprints. We need to create the right conditions for them to thrive if we wish to stay healthy.
Gut microbes perform many crucial functions like aiding digestion, producing vitamins, protection from harmful bacteria, keeping the gut healthy and intact, and preserving immunity.
While we can all harbour harmful gut microbiota, many experts believe that healthy people carry particular species, and combinations of species, of gut microorganisms.
Many signs indicate poor gut health, and only some of them are listed here. Other indications for assessing and addressing gut imbalance can include (but are not exclusive to) chronic illness, ongoing fatigue, recurring acute illnesses such as coughs, colds and flu, poor sleep and brain fog.
Here are some signs of an unhealthy gut.
1) Depression, anxiety and stress
We now know that there is a bidirectional gut/brain connection, meaning your gut health can affect your brain function and vice versa. This is known as the gut/brain axis.
It is not uncommon to find that a person suffering from mental health issues can also have a significant gut disturbance.
It works the other way around too, where someone with persistent digestive problems can also be experiencing chronic stress, anxiety or depression.
One study involving 668 students revealed chronic stress as a significant predictor of gastrointestinal disorders.
Gut microbes also manufacture chemicals linked to low mood or depression, such as serotonin. It’s commonly thought that low levels of serotonin in the brain are directly related to depression. But new research suggests that gut-based serotonin has a substantial impact on mental health.
If your gut health is impaired, the chances are that your digestive serotonin could be too, and this might be contributing to your depression.
2) Autoimmune disease
There are over 80 autoimmune diseases, including rheumatoid arthritis, psoriasis, lupus, Hashimoto’s thyroiditis, inflammatory bowel disease, Addison’s disease, Graves disease, multiple sclerosis, and Sjögren’s syndrome.
Damage to the finely-tuned gut microbiota and conditions such as leaky gut can lead to increased inflammatory processes in the body which compromise immunity.
In the case of autoimmunity, this leads to the immune system mistakenly attacking the healthy tissues and organs it is meant to protect.
Recently, researchers looked at the gut bacteria Enterococcus gallinarum, discovering that it can spontaneously locate outside of the gut to the lymph nodes, liver and spleen, causing an autoimmune response.
Other research also links the normal gut bacteria Bacteroides fragilis to autoimmune disease as it mimics a small protein called ubiquitin.
Not everyone produces this mimic protein (known as BfUbb), but for those who do, it can cause autoimmune dysregulation.
This highlights the importance of maintaining gut integrity and a healthy gut lining (mucosa) to block the passage of harmful substances into the bloodstream.
It also underlines the power gut bacteria holds to alter our immunity.
3) Allergies
Research supports the importance of the gut microbiome to protect against allergies by balancing our immune response to antigens. Without the right balance of healthy gut bacteria, we are less protected and more susceptible to allergic reactions.
Babies born by C-section have lower levels of some gut bacteria than those who pass through the birth canal, and this is linked to an increased risk of allergies, including asthma.
Maternal intake of antibiotics can also increase the risk of allergies in newborns and young children. Alterations in gut microbiota are also directly linked to food allergies.
To guard against allergies, you need to protect your gut health and cultivate a diverse yet balanced gut microbiota.
4) Eczema or other skin complaints
GI inflammation and poor diet can cause leaky gut, where its protective mucosal lining is damaged. It allows substances to enter the bloodstream, causing inflammation, including skin conditions such as eczema.
According to Cochrane, people with eczema sometimes have inflammation in their gut. Changes in gut microbiota can be associated with eczema in children.
Particular gut bacterias such as Bifidobacterium, Megasphaera, Haemophilus and Streptococcus are abundant in healthy children, whereas the proliferation of different gut bacteria is seen in those with eczema.
For example, increased levels of the bacterias Faecalibacterium prausnitzii and Ruminococcus gnavus are found in the guts of children with eczema. These are associated with inflammation and the tendency towards allergic rhinitis, asthma and atopic dermatitis (eczema).
While more evidence is needed, there is some research showing a link between gut permeability (leaky gut) and eczema in both children and adults.
There is also an apparent correlation between food allergies and eczema, and recent research suggests that the lack of certain gut bacteria is linked to this.
More studies are needed, but researchers reviewed recent findings linking eczema and gut microbiota. They determined that changes in the microbiome can contribute to the development, persistence and severity of the condition.
They also acknowledged a clear association between gut dysbiosis (microbial imbalance) and eczema.
5) Regular digestion issues

If you experience any recurring digestive problems or ongoing issues, this is a clear sign of poor gut health.
A healthy gut may have occasional disturbance, but should, on the whole, find it easy to digest and eliminate food.
There are many things you can do to address poor digestion, but it makes sense to start with your diet. Take a look at our article on all things digestion.
6) Unexplained weight changes
Weight loss can be a symptom of SIBO (Small Intestine Bacterial Overgrowth), a condition where there is an excessive amount of gut bacteria in the small intestine.
Gut issues can be one of the reasons why you might have weight gain or struggle to lose weight. For example, the microbiota has an influence over the regulation of metabolic activity, including weight and glucose control. When compromised, this can increase your risk of obesity and diabetes.
By digesting fibre, gut microbes also produce short-chain fatty acids such as butyrate and propionate. SCFAs improve both metabolic and appetite regulation and obesity.
In one study, propionate population of the colon modulated appetite by affecting the brain and lowering reward-based eating behaviour towards high energy foods.
As we already know, stress and anxiety can affect gut health. Poor gut health can lead to chronic inflammation, which can underlie obesity.
11 ways to improve poor gut health
1) Seek the advice of a nutritional therapist, naturopath or functional medicine practitioner
We are all unique. How we express symptoms and the solutions that we need for them vary from person to person. For example, it may be that you need to rest and repair your gut in other ways before taking probiotics.
Or perhaps one of the most useful things you can do to ease your symptoms is to manage your stress more effectively.
An accredited nutritional therapist, naturopath or functional medicine practitioner can give you the best advice and create an achievable, tailor-made plan to suit your needs. If necessary, they can also provide the most up to date and accurate testing to help decipher what is really going on with you.
2) Stop taking over-the-counter meds and unnecessary antibiotics
Drugs, in general, can affect the integrity of your gut microbiota. Aside from taking necessary prescription medication, it’s crucial to limit your intake of non-prescribed drugs.
For example, NSAIDs (non-steroidal anti-inflammatory drugs) such as Nurofen and ibuprofen, are known to impact the diversity of gut microbiome severely. Some NSAIDs have a more aggressive effect than others, such as naproxen and ketorolac.
According to gastroenterologist Byron Cryer, MD, a spokesperson for the American Gastroenterological Association, NSAIDs cause more than half of bleeding ulcers. They can also damage the mucosal gut barrier, leading to leaky gut.
Recently, researchers looked at the effect of antibiotics on oral infections. They found that antibiotics kill short-chain fatty acids produced by healthy gut bacteria, inhibiting the body’s ability to fight infection.
The researchers also found that if you leave those natural defences alone, they can effectively reduce inflammation and infection: so why kill them?
Several studies show the adverse effect of antibiotics on our gut and the potentially dire ramifications this can have on our immunity and overall health.
Some scientists even discuss the permanent damage antibiotics can have on our beneficial gut bacteria. Some friendly gut flora never fully recover, increasing our susceptibility to infection and disease.
One 2008 study looked at the gut bacteria of three healthy individuals before and after a single course of antibiotics. The drug, Ciprofloxacin, influenced one-third of their gut bacteria, decreasing the richness, diversity and evenness of the community.
There were individual variations among these, but in all three participants, after six months, several of the healthy gut bacteria failed to recover. This suggests that even a short course of antibiotics can detrimentally and perhaps permanently affect our gut health.
Where possible, try to find natural alternatives to pain, cough and cold relief, allergies, or any other reasons why you are turning to medication. If your doctor prescribes antibiotics, ask whether it is essential and if there are any alternatives.
3) Don't eat foods that aggravate your symptoms and clean up your diet
If you suffer from any digestive issues, cut out the foods you think could be aggravating your symptoms. You may also benefit from eliminating inflammatory foods such as dairy, grains, and gluten from your diet.
Sugar and sweeteners can also cause dysbiosis and inflammation, so it’s essential to cut down on sugar and most definitely eliminate sweeteners of any kind.
Cutting out processed and junk foods while increasing the amount and diversity of plant-based foods can significantly improve your gut health.
4) Eat daily pre and probiotic foods
Eating plenty of pre and probiotic foods will encourage a rich diversity of healthy gut bacteria. Add them daily to your meals to keep your gut healthy and strong.
Raw fermented foods are rich in probiotics and include full-fat natural yogurt, raw sauerkraut, gherkins, kefir or kombucha, miso and tempeh.
Prebiotic foods include garlic, leeks and onions (all three both raw and cooked), Jerusalem artichokes, cabbage, apples, under-ripe bananas, oats, beans and pulses, nuts and seeds.
5) Eat a diverse range of fruit, vegetables and fibre

A healthy gut contains a vast array of different microbiota. The more varied the species in your gut bacteria, the more potential health benefits you can gain and the stronger your gut wall.
By eating a diverse range of foods, especially plant foods, you will encourage this.
Ensure you eat a wide range of fruit and vegetables in all their different colours, consume lots of omega-3 fats, nuts and seeds, legumes, and pulses.
Fibre also makes your gut bacteria thrive. It speeds up the transit time of your food and creates a gut-friendly environment by removing toxins and improving constipation.
Fibre will also encourage short-chain fatty acid production to impact immunity, while also regulating your weight and glucose levels.
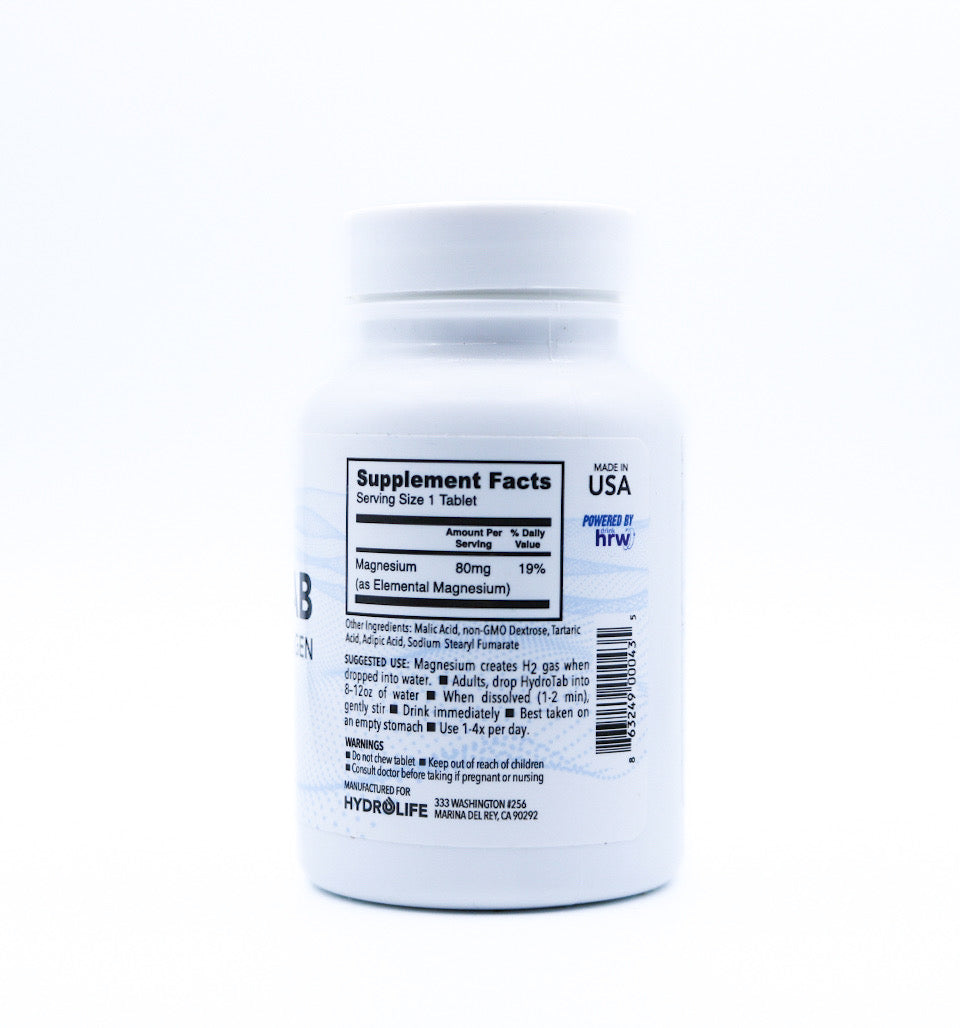
6) Work on your pH balance
Many practitioners recognise the importance of acid/alkaline balance in the blood. This is because illness and disease are less able to thrive in a less acidic environment.
Poor gut health promotes excessive acidity, but it’s not just about blood pH. It’s also essential to maintain a healthy pH throughout your GI tract. Without it, you cannot manage the intricate balance of microbiota and digestive enzymes needed for a well functioning gut.
You are also less able to absorb all the necessary nutrients from your food, and as we know, compromised gut integrity leads to inflammation, reduced immunity and increased susceptibility to disease.
One way to help keep your acid/alkaline balance in check is to add more alkaline foods to your diet. Ditch processed and junk foods, pre-prepared meals and sugar. Reduce your caffeine and alcohol intake. Some people may also find it beneficial to avoid dairy and cereal grains.
You could also take a daily green powder containing alkalising superfoods such as spirulina, chlorella, sprouts, and grasses.
pH balancing supplements can optimise stomach acid/alkaline levels and promote gut health. A natural one containing electrolytes can address this.
7) Take probiotics
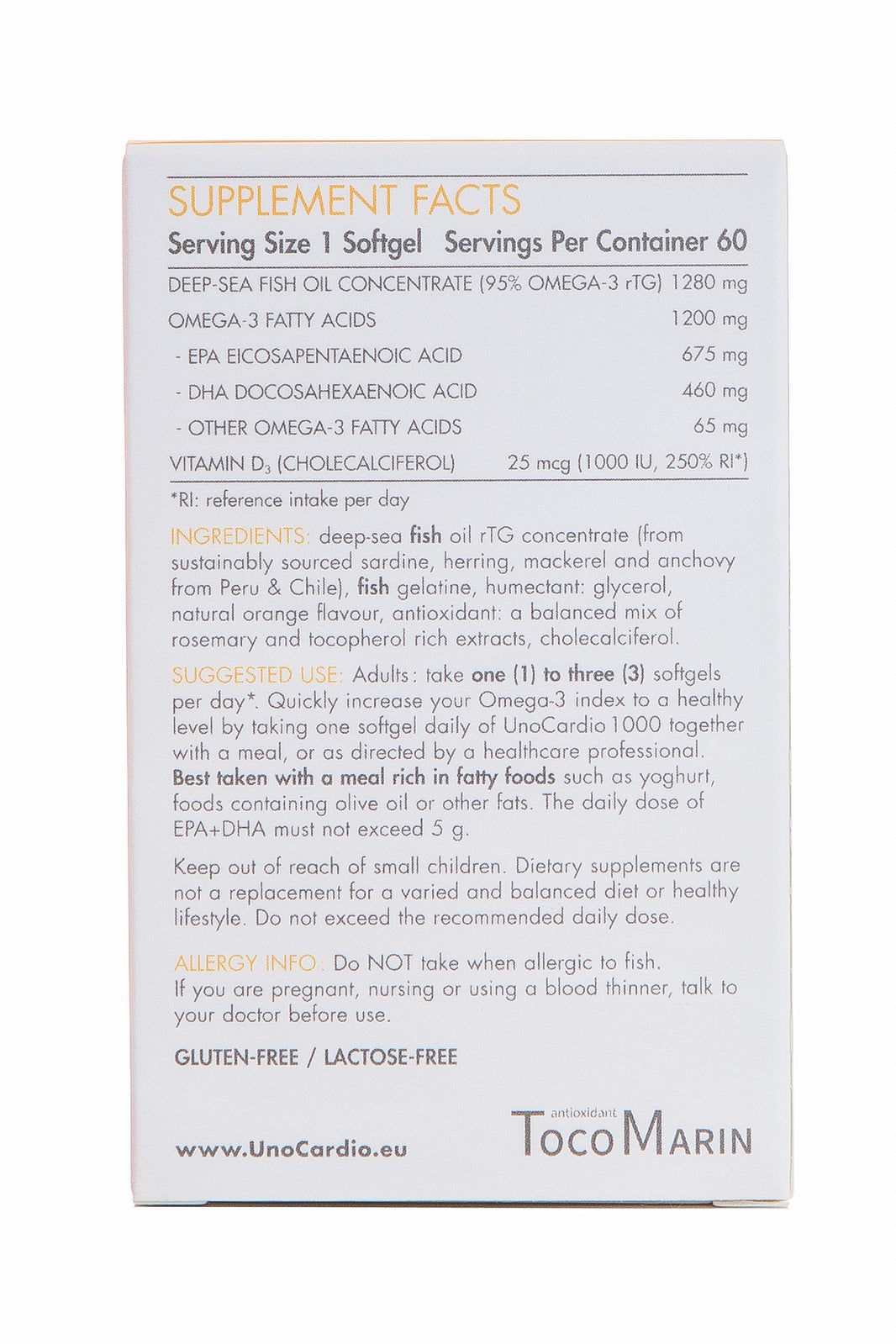
Probiotics are live, friendly bacteria that provide health benefits for you and your gut when taken in adequate amounts. They can be useful when your microbiota is out of balance and could do with a boost of the good stuff.
Opinions differ, but many experts believe that stronger is better when it comes to taking a probiotic supplement. The majority of probiotics you’ll find on the shelves come from bovine sources which are not indigenous to us.
So, for the most profound benefits, it makes sense to take a high-strength supplement derived from human bacterial strains.
Progurt is one of the most advanced probiotics on the market. It’s clinically tested and has an exceptionally high, one trillion Colony-Forming Units to populate your gut.
What makes Progurt particularly progressive is that the bacteria derive from human probiotic isolates (HPIs).
Each Progurt probiotic sachet contains HPI identical to the strains found in a healthy gut from birth. Innate and non-transient, the human strains in Progurt feature a unique combination and ratio that have been specially chosen to colonise in your GI tract and replicate.
They include missing, colonising, upper and lower gut, fragile, synergistic, replicating, migrating, and birth strains.
Bovine probiotics tend to be more transient, whereas our bodies respond to these native HPI bacteria more instinctively and effectively. They remain established in your gut unless poor health or medication disrupt your healthy gut environment, and you need a maintenance dose.
8) Eat at mealtimes, chew your food properly
This is pretty obvious, but it’s something that so many of us don’t do. We often rush our meals and get distracted by watching TV, working or looking at our phones.
Ensure you are chewing your food correctly as this is an integral part of digestion. It helps to break everything down and eases the whole process.
Savour the flavour of your meals, take in the aroma, and engage with every mouthful. Always try to eat at a table and don’t wolf your food.
9) Manage stress
There is a direct link between stress and GI disorders and studies support the benefits of stress-reducing interventions for this.
Evidence suggests that cognitive behavioural therapy, hypnosis and relaxation techniques can all significantly improve GI symptoms. Some studies also support the use of mindfulness, meditation and yoga for reducing IBS symptoms.
If you regularly struggle with stress or anxiety, make it your mission to find ways to alleviate the strain. This could be anything from being in nature, spending quality time with friends and loved ones, journaling or writing a daily gratitude diary, finding a hobby, getting involved in your community, practising deep breathing, exercising, or meditating.
The list goes on, but find the most effective forms of stress relief for you.
10) Get enough sleep
Sleep and gut health are connected, with one affecting the other.
A 2014 animal study demonstrated the harmful impact sleep disturbance might have on healthy gut bacteria. A small study with healthy male participants also found that as little as two nights disturbed sleep can noticeably alter the gut microbiota.
This is most likely related to the fact that, rather like the rest of you, your microbiota are programmed to regular circadian sleep-wake cycles and patterns of eating.
When this gets disrupted, your microbial health can suffer. This could be particularly problematic for frequent long-haul flyers and shift workers.
Aim for seven to eight hours of undisturbed sleep per night.
11) Exercise
Exercise and regular movement can help to shift food through your digestive tract.
Walking is an excellent form of exercise that is suitable for all levels of fitness as you can take it at your own pace.
If you have a job where you’re sitting down for much of the time, or you live a sedentary lifestyle, get up and move around at frequent intervals throughout your day.
Conclusion
There are several signs which can suggest your gut health is compromised, and while we have listed some of the major ones, there are others.
The steps mentioned in this article could make a significant improvement to any gut symptoms you are experiencing. They can also be useful for preventing gut problems – full stop.
However, depending on your issues, you may benefit more from a tailor-made solution. In this case, it’s best to seek the advice of a qualified professional who specialises in nutrition and holistic health, such as a nutritional therapist, naturopath or functional medicine practitioner.
This article is written by Rebecca Rychlik-Cunning, Nutritional Therapist and Homeopath. Follow Rebecca on Instagram, Facebook and Medium, @rebeccabitesback.
Water for Health Ltd began trading in 2007 with the goal of positively affecting the lives of many. We still retain that mission because we believe that proper hydration and nutrition can make a massive difference to people’s health and quality of life. Click here to find out more.























Leave a comment